
ACLS In-Hospital Cardiac Arrest in Pregnancy Algorithm
ACLS for Maternal Cardiac Arrest: In-Hospital Algorithm & Critical Steps
The sudden stop of effective circulation and breathing in a pregnant or postpartum woman, typically within 6 weeks of delivery in a hospital setting, is known as Maternal Cardiac Arrest (MCA) in-hospital. It requires immediate action to restore the mother’s heartbeat and prevent a lack of oxygen to the baby. Unlike typical cardiac arrest, pregnancy brings unique challenges such as aortocaval compression, rapid hypoxia, difficult airways, and the urgent need to save two lives at once. Doctors and nurses quickly begin chest compressions, give oxygen, and use medicines to restart the heart. If the heart doesn’t restart within 4-5 minutes and the pregnancy is 20 weeks or more, an emergency C-section may be performed right there to help save both the baby and the mother. Without fast, specialized care, outcomes can be devastating for both.


According to the National Institutes Of Health 2023 March 14 Among 10 921 784 U.S. delivery hospitalizations, the cardiac arrest rate was 13.4 per 100 000. Of the 1465 patients who had cardiac arrest, 68.6% (95% CI, 63.2% to 74.0%) survived to hospital discharge.
Why is the standard ACLS algorithm important? The answer lies in pregnancy’s physiologic changes demanding left uterine displacement, early perimortem C-section, and modified resuscitation tactics. This is why specialized maternal ACLS protocols are not just beneficial, they’re lifesaving.
Most Common Cause Of Cardiac Arrest In Pregnancy
Cardiac arrest during pregnancy is a rare but serious event, and it can occur due to several factors. Here are the main causes and other causes too:
Main Cause:
Hemorrhage:
- Severe blood loss during pregnancy or childbirth can lead to cardiac arrest.
Amniotic Fluid Embolism:
- Amniotic fluid entering the mother's bloodstream can trigger a severe, life-threatening reaction.
Pre-eclampsia/Eclampsia:
- High blood pressure complications can cause seizures and cardiac arrest in pregnant women.
Pulmonary Embolism:
- A blood clot blocking the lung arteries can rapidly stop the heart.
Aortic Dissection:
- A tear in the aorta’s wall can lead to sudden cardiovascular collapse.
Heart Failure:
- The heart's inability to pump blood effectively can cause arrest during pregnancy.
Sepsis (Blood Infection):
- A severe body-wide infection can lead to organ failure and cardiac arrest.
Other Causes:
Cardiac arrest in pregnant women can also result from trauma, severe allergic reactions, drug toxicity, and complications related to anesthesia.
Key Physiological Considerations in Pregnancy
Pregnancy brings about significant physiological changes that support the developing fetus and prepare the mother for childbirth. Understanding these adaptations is essential for providing safe and effective care during pregnancy and delivery.
1. Maternal Anatomical and Physiological Changes Affecting Resuscitation:
I. Cardiovascular Changes (Heart & Blood)
- More blood in the body — blood volume increases by about 30–50%.
- Heart rate gets faster — usually increases by 10–20 beats per minute.
- Lower blood pressure in early pregnancy, but it can increase later.
Why this matters:
The heart works harder, and blood pressure can drop easily when lying flat on the back because the growing uterus presses on a large blood vessel (the vena cava), reducing blood flow back to the heart.
II. Respiratory Changes (Breathing)
- Oxygen needs go up — the pregnant body and baby need more oxygen.
- Lungs have less room to expand because the uterus pushes up against them.
- Airway swelling makes it harder to insert a breathing tube.
Why this matters:
-The mother can run out of oxygen faster if her breathing stops.
-It can be trickier to manage her airway during resuscitation.
III. Metabolic Changes
- Faster metabolism — drugs may work differently or wear off faster.
- Blood sugar changes can affect how the body responds to emergencies.
Why this matters:
-Medications used during resuscitation might need adjusting.
-The baby’s health can also be affected by drugs given to the mother.
2. Impact on Chest Compressions, Airway Management, and Medicine Use:
I. Chest Compressions
- Tilt the mother to the left (15–30°) to prevent the uterus from pressing on the vena cava. Or manually move the uterus to the side while doing compressions.
- This helps keep blood flowing properly during CPR.
II. Airway Management
- Pregnant women’s airways are swollen and more sensitive.
- It can be harder to insert a breathing tube, so experienced hands, and smaller equipment might be needed.
- Give oxygen early and quickly, because the mother’s oxygen runs low faster.
III. Medicine Use
- Most medicine amounts (doses) stay the same, but the way the pregnant body handles medicines can change.
- Always think about the safety of both the mother and baby when choosing and giving medicines.
- Some medicines might need special care in timing or selection to avoid affecting the baby.
Perimortem Cesarean Delivery (PMCD)
- PMCD is an emergency cesarean performed during maternal cardiac arrest.
- It aims to improve both maternal resuscitation and fetal survival.
- Ideally performed within 4-5 minutes of cardiac arrest.
- Relieves aortocaval compression, enhancing maternal venous return.
- Indicated in pregnancies 20 weeks of gestation/5 months pregnant (uterine height at or above the umbilicus).
- Requires rapid, coordinated, multidisciplinary team response.
- The decision to perform PMCD depends on individual circumstances, including the fetus’s gestational age, the mother’s clinical status, available resources, and the expertise of the medical team.
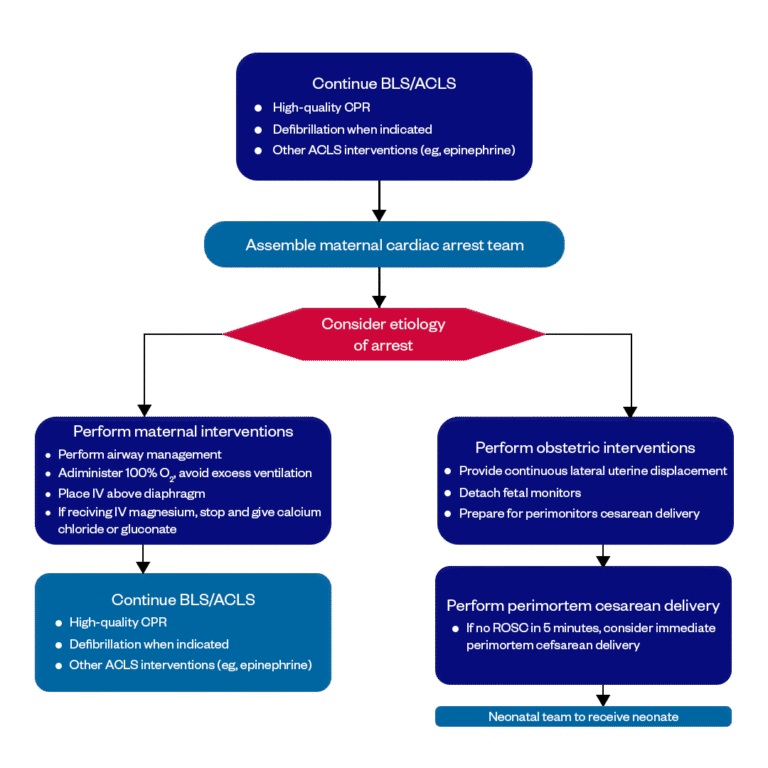
Cardiac Arrest in Pregnancy: In-Hospital ACLS Algorithm
Cardiac arrest during pregnancy is a rare but life-threatening emergency that requires rapid, specialized care. The In-Hospital ACLS Algorithm for pregnancy guides healthcare teams with clear, step-by-step actions to manage the mother’s cardiac arrest while considering the baby’s safety.
Cardiac arrest during pregnancy is a rare but life-threatening emergency that requires rapid, specialized care. The In-Hospital ACLS Algorithm for pregnancy guides healthcare teams with clear, step-by-step actions to manage the mother’s cardiac arrest while considering the baby’s safety.
01.
Continue BLS/ACLS
ACLS begins with high-quality CPR ( cardiopulmonary resuscitation) to keep blood flowing to the heart and brain. If needed, an advanced external defibrillator (AED) is used to deliver a shock for life-threatening heart rhythms such as ventricular fibrillation (V-fib) and pulseless ventricular tachycardia (pulseless V-tach). Medications like epinephrine are given to help restart the heart and improve blood flow. Other advanced interventions, such as securing the airway and monitoring heart rhythms, are also part of ACLS care.
Assemble the maternal cardiac arrest team
Quickly assemble a maternal cardiac arrest team, including obstetric (a branch of medical science focused on childbirth and the related stages of pregnancy and postpartum), an anesthesiologist (a doctor specialized in pain management), neonatal, and critical care specialists, to provide coordinated, specialized care during resuscitation.
03.
Consider the etiology of the arrest
Identify and treat the possible etiology of the cardiac arrest, such as bleeding, blood clots, heart problems, or other pregnancy-related complications.
04.
Perform maternal interventions
During maternal cardiac arrest, perform necessary interventions like airway management and securing an IV (intravenous) line above the diaphragm. Provide 100% oxygen while avoiding excessive ventilation. If the patient is receiving IV magnesium, stop the infusion and immediately give calcium chloride or calcium gluconate to counter its effects.
05.
Perform obstetric interventions
During maternal cardiac arrest, perform obstetric interventions by providing continuous lateral uterine displacement to relieve pressure on major blood vessels. Detach fetal monitors to focus on maternal resuscitation. If there’s no return of circulation within 4 minutes, prepare for a perimortem cesarean delivery to improve both maternal and fetal outcomes.
06.
Continue BLS/ACLS
Continue BLS/ACLS by performing high-quality CPR to maintain circulation. Use defibrillation if indicated to restore a normal heart rhythm. Administer other ACLS interventions, such as epinephrine, to improve blood flow and support the heart
07.
Perform perimortem cesarean delivery
If the return of spontaneous circulation (ROSC) is not achieved within 5 minutes, consider performing an immediate perimortem cesarean delivery. This can improve the chances of survival for both the mother and the baby.
08.
Neonatal team to receive neonate
Ensure the neonatal team (A group of healthcare professionals specialized in caring for newborns, especially premature babies) is ready to receive the neonate immediately after delivery to provide resuscitation and stabilization as needed.
Management of Cardiac Arrest In Pregnancy
Managing cardiac arrest in a pregnant woman is more complex than other cardiac arrest cases. In this case, there are two patients for the resuscitation teams, both the mother and the fetus require special consideration during this situation.
Optimal Patient Positioning and Left Uterine Displacement (LUD)
During cardiac arrest in pregnancy, the patient should be positioned on a firm (solid and stable) surface with continuous Left Uterine Displacement (LUD) to relieve pressure from the enlarged uterus on major blood vessels. This improves blood flow to the heart and brain, supporting effective resuscitation. Fig1, Fig2, and Fig3 will describe this position clearly.
Figure 1:

Image Source: Simulation and Medicine
Fig 1 shows a pregnant patient positioned with a slight tilt while receiving chest compressions from above. At the same time, Left Uterine Displacement (LUD) is performed by pushing the uterus to the left side. This helps reduce pressure on major blood vessels, improving blood flow to the heart and making resuscitation efforts more effective.
Figure 2:

Image Source: Simulation and Medicine
Fig 2 shows Left Uterine Displacement (LUD) being performed from the left side of the patient. In this technique, the healthcare provider gently pushes the pregnant uterus to the left to relieve pressure on the large blood vessels, helping to improve blood flow and support effective resuscitation.
Figure 3:

Image Source: Simulation and Medicine
Fig 3 shows Left Uterine Displacement (LUD) being done from the right side of the patient. The healthcare provider uses one or both hands to gently push the uterus to the left, reducing pressure on major blood vessels and improving circulation during resuscitation.
Quick Recap: ACLS Guidelines For Pregnancy Cardiac Arrest In-Hospital Management
In summary, maternal Cardiac Arrest (MCA) is a rare but life-threatening emergency that can happen during pregnancy or in the first six weeks after delivery. Some of the main causes include severe bleeding, amniotic fluid embolism, and complications from pre-eclampsia. In these situations, the standard ACLS protocol needs to be adjusted to meet the unique needs of pregnant patients.
The best way to be ready for these emergencies is through regular training, reviewing the special considerations for maternal care, and participating in team-based code simulations. Keeping your ACLS certification up to date, especially with a focus on obstetric care, ensures you’re prepared when every second matters.
At Bayside CPR, we offer specialized ACLS course to help healthcare providers build the skills and confidence to manage these critical situations. Enroll today and be ready to make a difference when it counts most.
Frequently Asked Questions
Can defibrillation be safely performed in pregnant patients, and does it require any modification?
- Yes, defibrillation is safe during pregnancy and should never be delayed. No modification in energy levels is necessary. However, attention must be given to uterine displacement during resuscitation.
How does medication dosing differ during ACLS in pregnancy?
- Most ACLS medications (epinephrine, amiodarone, etc) are given at standard adult doses during maternal cardiac arrest. The focus is on ensuring effective circulation to both mother and fetus, rather than adjusting doses.
Who should perform a perimortem cesarean delivery (PMCD) if no obstetrician is available?
In an emergency, any trained physician should initiate PMCD within 4–5 minutes of maternal arrest without ROSC. It’s a resuscitative procedure prioritized for maternal benefit as well as fetal rescue.
How should fetal monitoring be managed during maternal cardiac arrest?
Fetal monitoring is not prioritized during active resuscitation. The primary focus is maternal resuscitation. Fetal assessment resumes after maternal stabilization or during post-resuscitation care.
Which statement is most correct about cardiac arrest in pregnancy?
The most correct statement about cardiac arrest in pregnancy is that airway management and oxygenation should be prioritized during resuscitation for a pregnant patient.
After CPR has been started, when would it be appropriate to stop?
- The appropriate time to stop CPR is when a patient shows a signal of life or starts normal breathing, moving, opening eyes, or making sounds.


