
PALS Bradycardia Algorithm
Bradycardia refers to a slow heart rate that falls below the normal range for a patient’s age. In children, this condition is often a sign of low oxygen levels (hypoxia) and can be a critical warning that may precede cardiac arrest, particularly in infants and young kids. It should be treated timely, particularly if associated with poor perfusion signs like weak pulses, altered mental status, or hypotension. In PALS (Pediatric Advanced Life Support), bradycardia is generally defined as a heart rate below the expected range for age. For example, a heart rate less than 100 bpm in infants, less than 80 bpm in toddlers, less than 70 bpm in school-aged children, and less than 60 bpm in adolescents.
The PALS Bradycardia Algorithm plays a critical role in guiding the rapid assessment and management of abnormally slow heart rates in pediatric emergencies. It assists healthcare providers in quickly identifying reversible causes and determining when to start interventions such as oxygen, chest compressions, or medication to stabilize the child’s condition. Effective team coordination is essential in emergencies to ensure timely, organized, and accurate patient care. It helps reduce errors, improve communication, and improve the overall outcome for critically ill patients.

Classifications of PALS Bradycardia
We classify PALS bradycardia into two types based on its underlying cause and physiological response.
Types | Primary Bradycardia | Secondary Bradycardia |
Definition | An underlying cardiac condition, like heart block or sick sinus syndrome. | It is caused by non-cardiac problems, such as hypoxemia, acidosis, or hypothermia. |
Reasons | Myocarditis, surgical injury, cardiomyopathy, and congenital heart defects. | Hypoxia, acidosis, hypotension, hypothermia, and medication side effects. |
Cure | Cured by involving medication like atropine or placement of a permanent pacemaker. | Cured by treating causes like giving oxygen, correcting acidosis, or managing temperature. |
Note: In children (infants and babies, especially premature babies), secondary bradycardia is more common than primary bradycardia. This simply means that the sinus node is firing at a slow rate. It is caused by something outside of the heart.
Importance of the PALS Bradycardia Algorithm
The PALS Bradycardia Algorithm helps healthcare providers quickly recognize and treat dangerously slow heart rates in children. Here’s why this algorithm is so important:
- The PALS bradycardia algorithm offers clear, life-saving steps to boost heart function and protect vital organs.
- The algorithm helps healthcare providers manage bradycardia quickly and accurately, stopping it from progressing to cardiac arrest and greatly boosting survival rates.
- The pediatric bradycardia algorithm guarantees that healthcare providers follow consistent, evidence-based steps, even in high-stress, critical situations.
- It helps healthcare providers quickly decide when to escalate care, start CPR, or give medicines like epinephrine and atropine.
Key Considerations in The PALS Bradycardia Algorithm:
1. Assess and support ABCs:
- Act quickly to check the child’s airway, breathing, and circulation so you can stabilize their crucial signs and keep them pediatric secure.
2. Recognize Bradycardia:
- Watch for a heart rate that's slower than normal for the pediatric age, especially if they show signs of poor circulation or shock.
3. Identify the cause
- Check for probable causes of the bradycardia, like low oxygen levels (hypoxia), a drop in body temperature (hypothermia), exposure to toxins, or a heart block.
4. Initial Interventions:
- Give oxygen, make sure the child is breathing sufficiently, and start CPR if their heart rate drops below 60 beats per minute and they’re showing signs of insufficient circulation.
5. Advanced Interventions:
- If the bradycardia doesn’t improve with basic resuscitation, consider using medicines like epinephrine or atropine, or even pacing, if needed.
PALS Bradycardia Algorithm With a Pulse
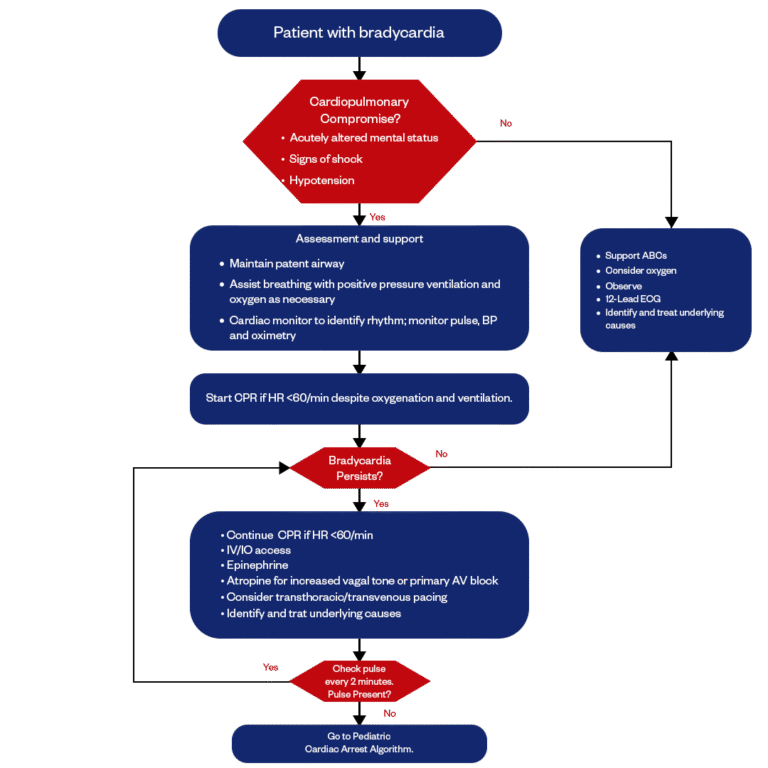
The PALS Bradycardia Algorithm with a pulse helps healthcare providers assess and manage pediatric patients who are experiencing slow heart rates but still have a pulse. It’s a critical tool for guiding treatment decisions to stabilize the child and ensure proper circulation while addressing the underlying causes of bradycardia.
01.
Identify Bradycardia
Bradycardia happens when a child's heart beats slower than what's normal for their age. It's important to catch it early and take the right actions to address it.
02.
Assess for Cardiopulmonary compromise?
When evaluating a patient with bradycardia, it is essential to evaluate for signs of cardiopulmonary compromise. Key indicators include acutely altered mental status, such as confusion, boredom, or unresponsiveness; signs of shock, like cold skin or body, delayed capillary refill, weak pulses, and poor perfusion; and hypotension, which indicates inadequate cardiac output. The presence of any of these signs alongside bradycardia suggests an unstable condition that requires immediate intervention to support airway, breathing, and circulation while identifying and treating the underlying cause.
- If signs are present, proceed to Step 3.
- If absent, proceed to Step 9.
03.
Support Airway, Breathing, and Circulation(ABCs)
During assessment and support, ensure the airway is patent and provide positive pressure ventilation and oxygen as needed. Use a cardiac monitor to assess the rhythm and continuously monitor vital signs, including pulse, blood pressure (BP), and oxygen saturation (SpO2). This helps guide further interventions and ensures optimal patient care.
04.
Evaluate Heart Rate
If the heart rate stays below 60 bpm even after providing oxygen and ventilation, begin CPR right away to help support circulation and stop things from getting worse.
05.
Determine if Bradycardia Persists
In kids, persistent bradycardia points to a serious underlying problem that needs quick attention. Acting fast with the right assessment and treatment is key to controlling complications and keeping circulation stable.
- If bradycardia persists, proceed to Step 6.
- If resolved, proceed to Step 9
06.
Administer Medications and Consider Pacing
If a patient experiences a heart rate less than 60 bpm, continue CPR. Establish intravenous (IV) or intraosseous (IO) access for medication administration. Administer epinephrine to help support circulation, and consider atropine if the issue is due to increased vagal tone or primary AV block. If necessary, consider transthoracic or transvenous pacing to restore a normal heart rate. Finally, it’s crucial to identify and treat any underlying causes contributing to bradycardia.
07.
Reassess Pulse Every 2 Minutes
Check the patient’s pulse every 2 minutes to keep an eye on their circulation and look for any changes.
- If a pulse is present, return to Step 5.
- If a pulse is not present, proceed to Step 8
08.
Go to Pediatric Cardiac Arrest Algorithm
If a pulse is not present, the healthcare provider should continue with the step-by-step approach outlined in the Pediatric Cardiac Arrest Algorithm. This includes delivering high-quality CPR, performing early defibrillation if a shockable rhythm is identified, and administering epinephrine promptly.
09.
Monitor and Support ABCs in Cardiac Care
Support the ABCs: Airway, Breathing, and Circulation. If the patient needs it, go ahead and give oxygen, and keep a close eye on how they're doing. It’s also important to run a 12-lead ECG to check their heart rhythm. From there, try to quickly pinpoint and treat whatever’s causing the problem, so you can stabilize the patient and decide on the next steps.
Medication Therapy for Bradycardia In Pediatrics
Medications for managing bradycardia in children are all about boosting the heart rate and stabilizing circulation. Each medication has a key role in handling specific situations.
1. Atropine
This medicine helps to speed up the heart rate when it’s too slow. It works by blocking certain signals that slow the heart down, allowing the heart to beat faster. Atropine IV/IO dose: 0.02 milligram per kilogram. May repeat once. The minimum dose is 0.1 mg, and the maximum single dose is 0.5 mg.
2. Epinephrine
Epinephrine is a medicine used when the heart rate is very slow and atropine doesn’t work. It helps by making the heart pump stronger and faster, and it also improves blood flow to vital organs. Epinephrine IV/IO dose: 0.01 milligram per kilogram (0.1 milliliter per kilogram of the 0.1 mg per ml concentration). Repeat every 3 to 5 minutes. If IV/IO access is not available but an endotracheal tube is in place, you may give an endotracheal tube dose of 0.1 mg per kilogram (0.1 ml per kilogram of the 1 mg per ml concentration).
3. Dopamine
Dopamine is a medication that helps to improve the heart’s ability to pump blood when the heart rate is low. It also supports blood pressure, ensuring that blood gets to all parts of the body, especially important organs like the brain and kidneys.
Note: Healthcare providers give these medications in different situations based on the severity of the bradycardia (slow heart rate) and the child’s response.
PALS Bradycardia Algorithm Critical Role in Pediatric Emergency Care
In short, the PALS Bradycardia Algorithm is key in quickly assessing and managing bradycardia in kids. It helps healthcare providers identify reversible causes of slow heart rates, preventing cardiac arrest. The algorithm guides clinicians through checking airway, breathing, and circulation, and outlines steps like starting CPR if the heart rate drops below 60 bpm and giving medications like atropine and epinephrine. By providing a clear, structured approach, the PALS Bradycardia Algorithm improves outcomes and survival rates for critically ill children.
Want to sharpen your pediatric emergency skills? Join our hands-on PALS certification course at Bayside CPR and become the confident, life-saving provider every child deserves.
Frequently Asked Questions
What is the IV/IO dose of atropine for pediatric bradycardia?
- The IV/IO dose of atropine for pediatric bradycardia is 0.02 mg/kg. This dose may be repeated once. The minimum quantity is 0.1 mg, and the maximum single quantity is 0.5 mg.
When should pediatric bradycardia be used with a pulse algorithm?
- The pediatric bradycardia with a pulse algorithm can be used when a child has bradycardia, exhibited by a slow heart rate with a pulse, and shows signs of cardiopulmonary compromise or instability.
What are the signs and symptoms of bradycardia in a pediatric patient?
- In children, bradycardia, or a slow heart rate, can show up with various symptoms like tiredness, weakness, dizziness, and trouble breathing. If the heart rate drops significantly, it can lead to more serious signs such as fainting, confusion, and even chest pain.
What initial assessments should be performed in a child with bradycardia?
- In a child with bradycardia, initial assessments should be checking the airway, breathing, circulation, and level of consciousness. Additionally, it’s crucial to specify any reversible causes, such as hypoxia or electrolyte imbalances.
What are the long-term considerations for a child after an episode of bradycardia?
- Long-term considerations for a child after an episode of bradycardia include regular monitoring by healthcare providers, care for underlying conditions, and potential activity modifications. Caregivers should also be educated on recognizing symptoms and understanding medication management, if applicable, to ensure the child’s ongoing health and safety.


