
Acute Coronary Syndrome (ACS)
Understanding Acute Coronary Syndrome (ACS)
Most heart attacks don’t happen suddenly or dramatically like we often see in movies. Instead, they commonly begin with subtle signs like mild discomfort, unusual pressure, or shortness of breath that gradually intensify. This slow and quiet onset is what makes Acute Coronary Syndrome (ACS) particularly dangerous. Because the early symptoms can be vague or easy to ignore, many people miss the chance to seek help before the situation becomes critical.

What Is Acute Coronary Syndrome?
ACS is a medical emergency that requires immediate attention. It refers to a range of conditions associated with sudden, reduced blood flow to the heart. The most serious form is a heart attack, but all types of ACS pose serious risks if not treated quickly.
Patients who have experienced ACS often describe it as a feeling of pressure, tightness, or a heavy weight on the chest. However, it’s important to understand that symptoms can show up differently from person to person. Some people can feel pain radiating to the arm, neck, jaw, or back, and others can experience cold sweats, nausea, or lightheadedness. In fact, 1 in 5 heart attacks are considered “silent”, meaning the person does not feel any chest pain at all. That’s why early recognition of the signs is critical.
Why Early Action Matters?
Every year, thousands of people rush to emergency departments with chest pain. Some walk in on their own, while others are carried in urgently. Regardless of how they arrive, the next 10 to 30 minutes are crucial. In that moment, recognizing ACS, starting appropriate treatment, and making the right clinical decisions can be the difference between survival and lasting heart damage or worse.
To help you better understand Acute Coronary Syndrome, we’ve created a clear and concise guide. It covers:
-The different types of Acute Coronary Syndrome
-Immediate actions and evidence-based treatment options
Whether you’re learning for your own health or for patient care, this guide provides essential knowledge of ACS in a straightforward way, empowering you to act quickly and confidently when it matters most.

Types of Acute Coronary Syndrome
Acute Coronary Syndrome isn’t a single condition—it’s a term that covers several problems related to reduced blood flow to the heart. That reduction is usually caused by a blockage in one or more coronary arteries, most often due to a blood clot.
There are three main types of ACS:
- ST-Elevation Myocardial Infarction (STEMI) – A major artery is completely blocked, and part of the heart muscle starts to die. It shows up clearly on an ECG.
- Non-ST-Elevation Myocardial Infarction (NSTEMI) – There’s still damage to the heart, but the blockage isn’t complete. The ECG may look normal or only slightly abnormal.
- Unstable Angina – This causes chest pain like a heart attack but without any actual heart muscle damage (yet). It’s still considered a medical emergency.
The ACS Response Algorithm: Step-by-Step Breakdown
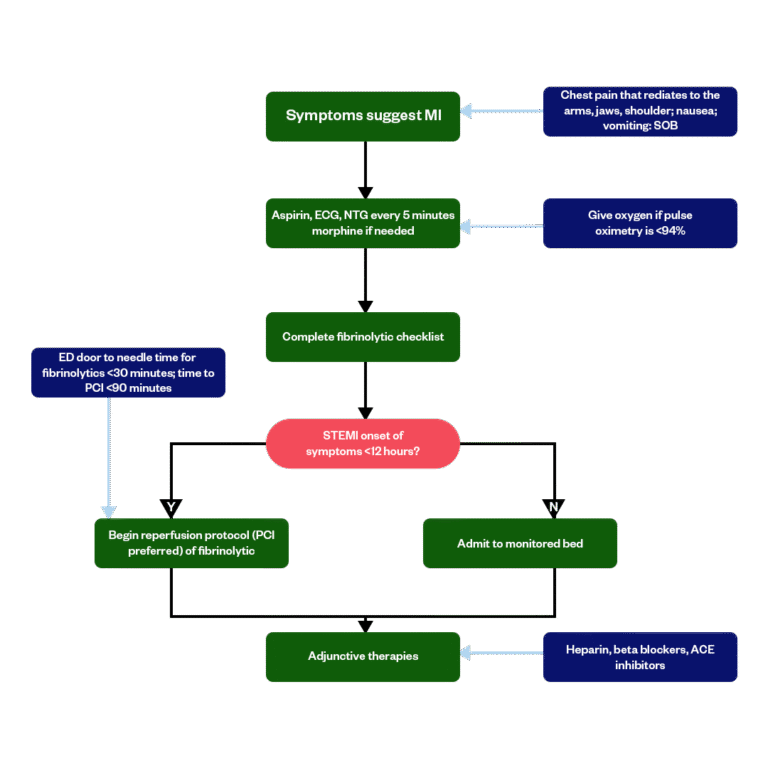
Knowing how to respond when ACS is suspected can save lives. Here’s a step-by-step look at what trained professionals do during an emergency—and why each step matters.
01.
Initial Evaluation
The first thing emergency teams do is assess the patient:
- Take a detailed medical history, including any risk factors like high blood pressure, diabetes, or a history of smoking.
- Perform a physical examination.
- Run a 12-lead ECG within the first 10 minutes of arrival. This test checks for patterns that suggest a heart attack is happening or has already started.
The ECG is one of the most important tools for determining what kind of ACS we’re dealing with.
02.
Immediate Treatment
Start the initial treatment as soon as you identify the type of ACS or even before all the test results are in:
- Give aspirin (300mg) immediately, usually to chew, to help prevent the clot from worsening.
- Use nitroglycerin to relieve chest pain by relaxing the blood vessels, but only if the patient's blood pressure isn't too low.
- Provide oxygen if blood oxygen levels fall below 90%.
- Use pain relief, such as morphine, in severe cases, but with caution.
03.
Confirming the Diagnosis
After stabilizing the patient, additional tests confirm the type of ACS:
- Troponin blood tests: These measure proteins that the heart releases when it’s damaged.
- Serial ECGs: Sometimes changes in the heart’s rhythm take time to show up, so ECGs are repeated.
- Imaging: Tests like echocardiograms or stress tests help spot blockages or weak spots in the heart muscle.
A STEMI diagnosis usually comes with clear ECG changes. For NSTEMI, diagnosis often depends on raised troponin levels without ST-elevation. Unstable angina presents like a heart attack but with normal test results.
04.
Risk Assessment
Once you confirm the type of ACS, find out how serious it is:
- Is the patient stable or unstable?
- Are dangerous heart rhythms present?
- Are symptoms ongoing?
Prioritize high-risk patients—those with persistent chest pain, low blood pressure, or signs of heart failure—for immediate procedures.
05.
Reperfusion: Opening the Blocked Artery
Treat STEMI patients with primary PCI (Percutaneous Coronary Intervention), commonly known as angioplasty, as the first-line approach. Aim to perform the procedure within 90 minutes of the patient’s arrival.
If you can't access PCI quickly, particularly in regional or rural settings, administer fibrinolytics (clot-busting drugs) instead.
For NSTEMI or unstable angina, assess the patient’s risk level. Provide urgent PCI for high-risk patients, and manage lower-risk patients with medication and close monitoring.
06.
Long-Term Medication and Monitoring
After the immediate crisis is managed, most patients will need ongoing medication to protect their heart and prevent future issues:
- Antiplatelet drugs (e.g. clopidogrel, ticagrelor) to stop new clots.
- Beta-blockers to reduce strain on the heart.
- ACE inhibitors or ARBs for patients with high blood pressure or heart failure.
- Statins to manage cholesterol levels.
- Patients are also monitored closely in a hospital setting, where their heart rhythm, oxygen levels, and symptoms are tracked 24/7.
07.
Recovery and Prevention
Once patients are out of immediate danger, the focus shifts to recovery and preventing another episode. This includes:
- You should recommend to patients to change their lifestyle, like quitting smoking, eating a heart-healthy diet, and staying active.
- Cardiac rehabilitation, which includes supervised exercise and education.
- Follow-up care with a GP or cardiologist.
- Medication adherence, since stopping meds too soon is a leading cause of repeat heart attacks.
Final Thoughts
When it comes to Acute Coronary Syndrome, the difference between a full recovery and lasting damage often comes down to how quickly you respond. Early signs can be subtle, and many people don’t recognize them until it’s almost too late. Understanding these signs and knowing what steps to take can save lives.
At Bayside CPR, we’re committed to delivering high-quality training that empowers everyday people and professionals to respond to cardiac emergencies with confidence and clarity. Whether you’re in the medical field or just someone who wants to be prepared, we offer the skills and knowledge to make a difference when it truly matters.
Want to be prepared to respond to a heart emergency?
Enroll in our next ACLS, BLS, or CPR certification course and gain life-saving skills you can trust.
Frequently Asked Questions
What is Acute Coronary Syndrome (ACS)?
ACS is a term used for situations where the blood supply to the heart muscle is suddenly blocked. This can range from unstable angina (chest pain without heart damage) to heart attacks like NSTEMI and STEMI, which do cause damage.
What is the first step in the ACS algorithm?
Immediate assessment of vital signs, obtaining a 12-lead ECG within 10 minutes, and initiating oxygen (if hypoxic), aspirin, and nitrates (if no contraindications).
What’s the difference between STEMI and NSTEMI in terms of treatment?
STEMI is a medical emergency — the artery is fully blocked, so doctors aim to open it quickly with a procedure called PCI (angioplasty). NSTEMI doesn’t always need immediate PCI but does require close monitoring and medications to reduce the risk of further damage.
What treatments are used in ACS cases?
Several medications play a role, including:
Aspirin and other antiplatelets to stop new clots
Blood thinners like heparin
Beta-blockers to slow the heart
Statins to manage cholesterol
Nitrates or morphine for pain and chest pressure


