
ACLS Bradycardia
Algorithm
According to the National Institutes of Health (NIH) Epub 2019 Jul 9, bradycardia is a resting heart rate of 50-60 beats per minute (bpm), which can be normal in some individuals, especially those who are young, physically fit, or during sleep, but can also indicate a medical condition. For most adults, a normal resting heart rate ranges from 60 to 100 beats per minute (bpm).

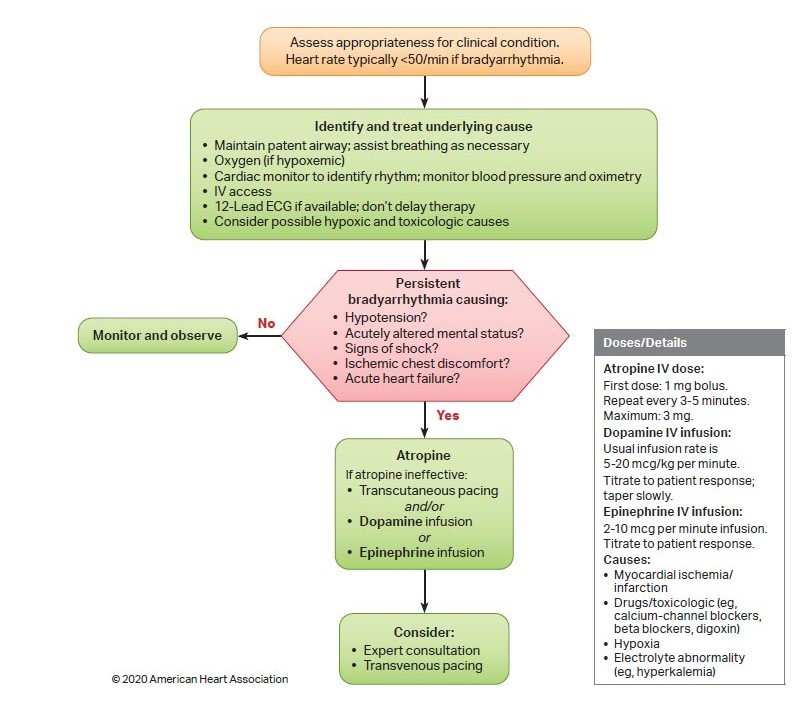
ACLS Bradycardia Algorithm is a component of Advanced Cardiac Life Support (ACLS) used in emergency care to treat patients experiencing bradycardia. This algorithm offers a step-by-step approach that begins with assessing the patient for symptoms and identifying possible causes of the slow heart rate. It includes ensuring the airway is clear, monitoring vital signs such as heart rhythm, blood pressure, and oxygen saturation, establishing IV (Intravenous) access, and administering appropriate treatments like atropine, transcutaneous pacing, or dopamine/epinephrine when necessary.
It’s a structured step-by-step strategy healthcare professionals use to handle slow heart rates effectively.
Symptoms Of Bradycardia
Bradycardia may not always cause noticeable symptoms, but when it does, they can include:
- The person may feel weak.
- When a person feels dizzy or light-headed
- Fainting (syncope) or near-fainting.
- Shortness of breath, problem in breathing
- Feeling discomfort or chest pain.
- Confused or can’t remember things (memory loss).
- Can't tolerate the day-to-day life exercise and movements.
- When a person feels cool, moist, and sometimes pale.
These symptoms occur because the heart is not pumping enough blood to meet the body’s needs. If these symptoms you are suspecting, immediate assessment and treatment are essential.
ACLS Bradycardia Algorithm Importance
It is important because it helps healthcare providers know what to do when a person’s heart rate is too slow and it’s causing serious symptoms.
- It gives step-by-step instructions to find the problem.
- Helps decide if the slow heart rate is dangerous.
- Guides when to give medication or use a pacemaker.
- Helps save lives by making sure the right treatment is given at the right time.
ACLS Bradycardia Treatment
Bradycardia treatment varies depending on the patient’s clinical conditions, symptoms, and the root cause of the slow heart rate. The focus is on managing symptoms and identifying the underlying issue using the Hs and Ts framework from the ACLS bradycardia algorithm. We’ll explore the Hs and Ts in more detail later, but first, let’s look at the basic technique for treating bradycardia.
01.
Airway, Breathing, and Circulation (ABCs):
Begin by assessing and stabilizing the patient's airway, breathing, and circulation. Provide necessary interventions as needed.
02.
Monitor Vital Signs:
Continuously check and document key vitals, including heart rate, blood pressure, and oxygen saturation.
03.
Identify the Underlying Cause:
Investigate and determine the root cause of the bradycardia. Potential causes include hypoxia, low blood volume, acidosis, toxic exposures, or intrinsic cardiac conditions such as heart blocks.
04.
Evaluate for Symptoms:
Differentiate between symptomatic and asymptomatic bradycardia. Symptoms such as chest pain, low blood pressure, altered consciousness, or signs of shock indicate hemodynamic instability and require prompt action.
05.
Atropine Administration:
If the patient shows signs of symptomatic bradycardia with poor circulation, administer atropine.
- The standard adult dose is 0.5 mg IV, which can be repeated every 3–5 minutes up to a maximum of 3 mg.
- Atropine is especially useful in cases related to vagal stimulation or certain drug overdoses.
06.
Consider Dopamine or Epinephrine:
If atropine fails or isn’t suitable, use dopamine or epinephrine to enhance heart rate and cardiac output:
- Dopamine infusion: 2–20 mcg/kg/min
- Epinephrine infusion: 2–10 mcg/min
07.
Temporary Pacing:
For severe bradycardia that doesn’t respond to medications or if the patient remains unstable, initiate transcutaneous pacing.
08.
Specialist Consultation:
When bradycardia is linked to cardiac conduction abnormalities such as heart blocks, consult a cardiologist or electrophysiologist. A permanent pacemaker may be required for long-term management.
Special Considerations in the Bradycardia Algorithm
Pediatric Patients:
- Bradycardia in children is often secondary to hypoxia.
- Prioritize airway management and oxygenation before pharmacologic interventions.
- Atropine dosing: 0.02 mg/kg IV (minimum dose 0.1 mg; max single dose 0.5 mg in children, 1 mg in adolescents).
Myocardial Infarction (MI):
- Bradycardia may result from inferior wall (Myocardial Infarction) MI(RCA Right Coronary Artery involvement).
- Use caution with atropine, as it may worsen ischemia.
- Prepare for pacing if a high-degree AV block develops.
Hypothermia:
- Bradycardia is expected in hypothermic patients and may be physiologic.
- Avoid atropine or pacing until core temperature is corrected (>30°C/86°F).
- Rewarm first before assuming pathologic bradycardia.
Beta-Blocker or Calcium Channel Blocker Toxicity:
- This may be resistant to atropine.
- Consider high-dose insulin therapy, glucagon, or calcium gluconate depending on the agent involved.
- Lipid emulsion therapy can be considered in severe toxicity.
Do-Not-Resuscitate (DNR) or Advanced Directives:
- Always check what the patient wants and their care goals before starting serious treatments like pacing or moving them to the ICU.
High-Degree AV(Atrioventricular) Block:
- Second-degree type II or third-degree AV blocks typically require pacing rather than atropine.
- Treat as unstable until proven otherwise.
Medication Considerations:
- Monitor for cumulative effects of sedatives, opioids, or digoxin, which may contribute to bradycardia.
- Consider drug levels/toxicology screening if appropriate.
Heart Transplant Patients:
- Atropine may be ineffective due to denervation of the heart.
- Direct pacing or chronotropic agents like isoproterenol (isoprenaline) may be more effective.
Hs and Ts of ACLS Bradycardia Algorithm
| Possible Causes | How To Recognize | Treatment |
| Hypovolemia | Fast heart rate with a narrow QRS on ECG, along with signs of low blood volume. | Infusion of normal saline or Ringer’s lactate |
Hypoxia | Heart rate will be slow | Airway management and successful oxygenation |
Hydrogen Ion Excess (Acidosis) | Low QRS voltage on an ECG | Rapid breathing; consider giving a bolus of sodium bicarbonate |
Hypoglycaemia | Bedside glucose monitoring | Intravenous (IV) bolus of dextrose |
Hypokalaemia | Flat T waves and the appearance of U wave on the ECG | Intravenous (IV) magnesium infusion |
Hyperkalaemia | Peaked T waves and wide QRS complex on the ECG | Think about giving calcium chloride and sodium bicarbonate, along with starting an insulin and glucose protocol |
Hypothermia | Exposure to a cold environment | Gently rewarming |
Tension Pneumothorax | Heart rate will be slow and insufficient QRS complexes on the ECG; uneasy in breathing | Needle Decompression or Thoracostomy |
| Tamponade (cardiac) | Heart rate will be fast and insufficient QRS complexes on the ECG; uneasy in breathing | Pericardiocentesis (Pericardium) |
| Toxins | Usually present with a prolonged QT interval on ECG and may be accompanied by neurological symptoms | Based on particular toxins |
Thrombosis (pulmonary) | Heart rate will be fast with insufficient QRS complexes on the ECG | Perform a surgical embolectomy or administer fibrinolytic therapy |
Thrombosis (myocardial infarction) | The ECG will show abnormalities corresponding to the location of the infarction | It depends on the severity and timing of the myocardial infarction (MI) |
Final Thoughts on Managing Bradycardia in ACLS
Effective management of bradycardia under ACLS guidelines is crucial for optimizing outcomes in emergencies. Quickly noticing the problem, finding out what’s causing it, and giving the right treatment, like medicine or pacing, can help stop the patient from getting worse. Regular training and following up-to-date guidelines help medical teams stay ready to act fast and handle situations well. A systematic approach to bradycardia not only saves lives but also strengthens overall cardiovascular care.
Frequently Asked Questions
What is the first intervention for bradycardia?
The first steps in managing bradycardia include securing the airway and supporting breathing, providing continuous monitoring, administering oxygen as needed, assessing blood pressure and oxygen saturation, and establishing intravenous (IV) access. It’s also essential to obtain an ECG to accurately assess and monitor the heart rhythm.
When is the ACLS Bradycardia Algorithm used?
It is used when a patient has symptomatic bradycardia, meaning their slow heart rate is causing symptoms like hypotension, dizziness, or altered mental status.
How does epinephrine or dopamine help in bradycardia?
These medications act as vasopressors, increasing heart rate and blood pressure when atropine is ineffective.
What should be monitored during treatment?
Continuous ECG, blood pressure, oxygen saturation, and patient response to interventions should be closely monitored.
Is CPR Given for Bradycardia?
CPR is not typically given for bradycardia unless the patient has no pulse or is unresponsive . If this situation arises, CPR must be started immediately, and the ACLS cardiac arrest algorithm should be followed.
When is transcutaneous pacing (TCP) recommended?
TCP is recommended if the patient has severe symptoms (e.g., shock, or altered mental status) and does not respond to atropine.
How do you stabilize bradycardia?
Bradycardia can be stabilized using medications such as atropine, dopamine, or epinephrine, and may also require a temporary pacemaker to help regulate the heart rate.


