
ACLS Cardiac Arrest Algorithm
When cardiac arrest strikes, it often happens without warning, and quick action can make all the difference between life and death. Cardiac arrest is the sudden and unexpected failure of the heart’s ability to pump blood, leading to loss of consciousness, no normal breathing, and no signs of circulation. According to the American Heart Association, cardiac arrest is a leading cause of death in the United States, with over 350,000 out-of-hospital cardiac arrests occurring annually.
For more insights on factors affecting survival rates, explore our gender differences in cardiac arrest outcomes.
One of the most effective ways to handle these high-stakes situations is by utilizing Advanced Cardiovascular Life Support (ACLS). The ACLS Cardiac Arrest Algorithm is a set of advanced cardiovascular life support guidelines, specifically for managing and treating patients during cardiac arrest events. ACLS equips healthcare providers with the skills and knowledge to respond swiftly and systematically in emergencies, particularly during cardiac arrest. No matter where you are—whether in a hospital, in an ambulance, or even out in public places—knowing the ACLS Cardiac Arrest Algorithm allows you to respond quickly, based on proven guidelines.
This guide will break down the ACLS Cardiac Arrest Algorithm, starting with the basics, so you can fully understand and confidently apply it when needed.

ACLS Cardiac Arrest Algorithm: A Step-by-Step Breakdown
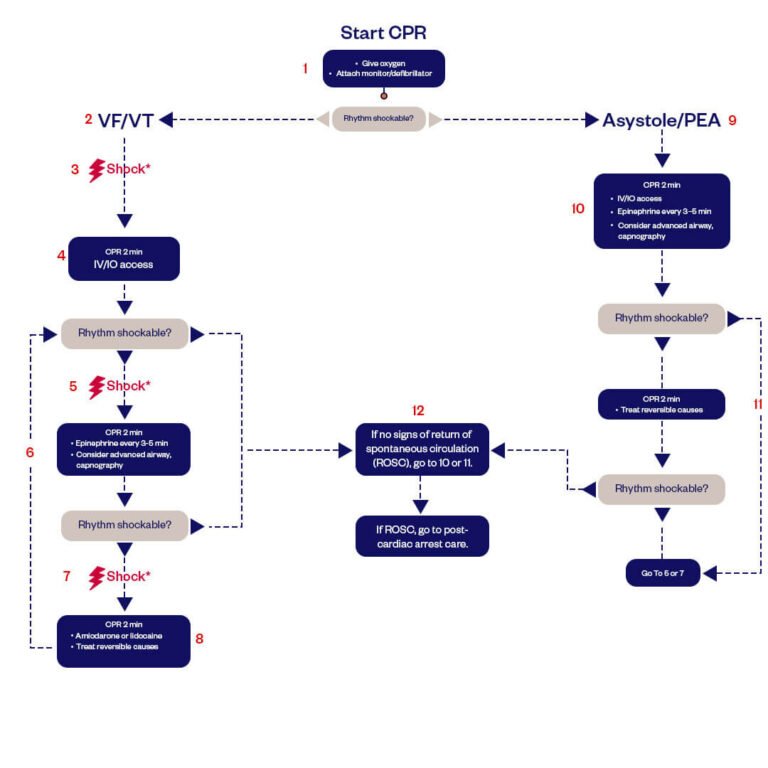
By following a systematic sequence of actions, you can make rapid decisions under pressure. The algorithm consists of several key steps:
1. Start CPR:
You should perform high-quality chest compressions at a rate of 100 to 120 per minute, allowing the chest to recoil. You should get the oxygen onboard and attach a monitor or defibrillator. Then, you should get back to chest compressions with minimal interruption and avoid overventilation, with a 30:2 compression-to-ventilation ratio if no advanced airway is in place.
2. Rhythm Analysis
You should assess whether the patient has a shockable (Ventricular Fibrillation [VF] or Pulseless Ventricular Tachycardia [pVT]) / non-shockable (Asystole or PEA) heart rhythm. You should not interrupt chest compressions for longer than 10 seconds during this assessment.
3. Management of Shockable Rhythms (VF/pVT):
- Immediate Defibrillation: If you see a shockable rhythm, charge the defib and continue chest compressions until it’s ready. Ensure all personnel are clear of the patient, then shock with an initial dose of 120 to 200 joules.
- Post-Shock CPR: Resume CPR immediately for 2 minutes and obtain IV/IO access.
- Reassessment: After 2 minutes of CPR, check the rhythm. If it is still shockable, give another shock.
- Medication Administration: Continue CPR for an additional 2 minutes. Give epinephrine every 3-5 minutes and consider advanced airway placement with capnography.
- Antiarrhythmic Drugs: If the rhythm remains shockable after delivered shocks, Antiarrhythmic drugs (e.g., Amiodarone, lidocaine) + reversible causes Hs Ts (Hypoxia, Hypovolemia, Hydrogen ion [acidosis], Hypo/Hyperkalemia, Hypothermia, Tension pneumothorax, Taponade, Toxins, Thrombosis [coronary or pulmonary]).
4. Management of Non-Shockable Rhythms (Asystole/PEA):
- Continuous CPR: If there is a non-shockable rhythm, continue quality CPR and establish IV/IO access.
- Epinephrine Administration: Administer epinephrine every 3-5 minutes.
- Advanced Airway and Capnography: You can place advanced airways and monitor end-tidal CO₂ to determine the effectiveness of CPR.
- Identify and Treat Reversible Causes: Guided by the Hs and Ts algorithm, investigate and address potentially reversible causes of the arrest.
5. Assess for Return of Spontaneous Circulation (ROSC)
Assess for return of spontaneous circulation after every 5 cycles. If ROSC + Restart cardiac therapy as indicated and begin post-cardiac arrest care. If not, continue the algorithm, reevaluating and treating reversible causes as appropriate.
Medications in ACLS
Epinephrine is a vasopressor that increases blood flow to vital organs and is administered every 3-5 minutes during a cardiac arrest. Amiodarone is the drug of choice for refractory VF/pVT, with an initial 300 mg dose and a second dose of 150 mg if needed. When Amiodarone is unavailable or ineffective, lidocaine can be used instead. When used alongside good CPR techniques and defibrillation, these medications help improve the odds of restoring circulation.
Advanced Airway Management
In certain situations, an advanced airway must be established for adequate oxygenation and ventilation. When Bag-mask ventilation is insufficient, endotracheal intubation or supraglottic airway placement is used. Capnography measures end-tidal CO2 (ETCO2), which confirms airway placement and monitors CPR effectiveness. A low ETCO2 reading of <10 mmHg indicates ineffective chest compressions or the need for additional interventions.
Reversible Causes of Cardiac Arrest
Identifying and treating reversible causes are vital steps in managing cardiac arrest. These are treatable conditions that are reversible and might increase the likelihood of patient survival if caught in time. We have the Hs and Ts framework for these reversible causes. These causes include:
Hs:
- Hypoxia: Insufficient oxygen in the blood.
- Hypovolemia: A Decrease in blood volume, particularly from bleeding or dehydration.
- Hydrogen ion (acidosis): Address with ventilation and sodium bicarbonate if indicated.
- Hyper-/hypokalemia: Use calcium chloride, insulin with glucose, or other electrolyte-balancing treatments.
- Hypothermia: Gradual warming strategies are crucial to prevent arrhythmias.
Ts:
- Tension pneumothorax: Perform immediate needle decompression followed by chest tube placement
- Tamponade (Cardiac Tamponade): Accumulating fluid around the heart that limits its ability to pump blood.
- Toxins: Drug overdose or contact with chemicals that can slow down heart function.
- Thrombosis (Coronary or Pulmonary): Conditions when blood clots form in the heart (coronary) or lungs (pulmonary), obstructing blood flow.
Recognizing and treating these reversible causes can make a marked difference in the resuscitation outcome. Detecting these factors in the early stages of the disease can steer treatment choices and even save lives.
Post-Cardiac Arrest Care
The successful resuscitation of a patient is just the beginning. The care of the patient after they have experienced cardiac arrest centers on three things: stabilizing the patient, preventing a recurrence, and limiting brain damage. A few measures, such as keeping blood pressure, oxygenation, continuous ECG monitoring, and learning ECG rhythms recognition and interpretation for ACLS, ensure proper recovery. Targeted Temperature Management (TTM) (or therapeutic hypothermia) reduces the risk of sustained neurological injury by maintaining and controlling a body temperature range between 32–36°C.
Conclusion
The ACLS cardiac arrest algorithm is a powerful guideline that helps healthcare providers make life-saving decisions during cardiac arrest situations. Rapid, informed decision-making, teamwork, and an in-depth understanding of current guidelines are crucial during resuscitation. As a healthcare professional, honing your skills through repeated practice and renewing your training can be the decisive factor when every second counts. Enroll in ACLS classes today and gain the confidence to take charge in an emergency. It’s not just a card — it’s your willingness to save a life.
Frequently Asked Questions
What is Cardiac Arrest Algorithm in ACLS?
ACLS cardiac arrest algorithm is a step-by-step protocol for dealing with cardiac arrest. It involves doing CPR, defibrillation, administering medications, and post-resuscitation care to improve the chances of survival.
How to Memorize ACLS Algorithms?
ACLS algorithms can be difficult to memorize. However, you can break them down into sections and use memory cues to remember key steps. Practicing through simulation and repetition can also help to reinforce the concepts.
What is the ACLS Algorithm ABCD?
The ACLS Algorithm ABCD stands for Airway, Breathing, Circulation, and Defibrillation. This phrase reminds health professionals of steps to take during cardiac arrest, from airway clearance to breathing, circulation, and defibrillation.
What is the CPR-to-Breath Ratio in ACLS?
In ACLS, the CPR-to-breath ratio for adults is 30 compressions to 2 breaths. If an advanced airway is in place, chest compressions should be continuous without a specific ratio of breaths.
Is it Possible to Fail ACLS?
Yes, it’s possible to fail ACLS if you do not demonstrate proficiency in performing required life-saving skills or fail the written and practical exams. Consistent practice and understanding of ACLS algorithms are essential to pass. However, ACLS through Bayside CPR guarantees that you’ll pass every single time.


