Pediatric Cardiac Arrest Algorithm
What if you witness a child suddenly collapse and stop breathing? It’s a terrifying thought, but one that could happen when you least expect it. Pediatric cardiac arrest occurs when a child’s heart stops pumping effectively, which means blood and oxygen are no longer reaching the brain and other vital organs. Time is critical in this situation.
Unlike adults, where cardiac arrest is often due to heart disease, in children, it’s usually the result of something like severe breathing problems or shock. That’s why early recognition and action are so important. The faster you respond, with high-quality CPR and emergency interventions, the better the probabilities of survival.
The PALS algorithm is more than just a checklist of medical steps; it’s a thoughtful, structured approach that helps healthcare providers think clearly and act quickly in high-pressure situations. Whether you’re in the emergency room, in an ambulance, or standing beside a young patient.

Recognizing Pediatric Cardiac Arrest
Identifying pediatric cardiac arrest quickly can significantly impact results. Below are key signs to look for:
- Sudden loss of consciousness, where the child is unresponsive and cannot be awakened.
- Absence of normal breathing or gasping breaths, indicating that the child is not getting enough oxygen.
- No pulse detected in the central areas of the kids body, such as the neck or groin.
- An unusually pale or bluish skin color (cyanosis), particularly around the lips, face, and extremities (limbs of the body such as arm,leg).
- The child may exhibit other signs of severe distress, such as seizures or abnormal movements, before collapsing.
Key Considerations
When handling pediatric cardiac arrest, several key considerations must be taken into account, including anatomical and physiological differences, team dynamics, and the importance of family support.
- Children aren't just small adults; their smaller airways, faster heart rates, and limited oxygen reserves make them more vulnerable to respiratory failure. Understanding these differences is essential for accurate estimation and effective treatment.
- Pediatric emergencies can be very stressful and move quickly. To work well as a team, everyone needs to communicate, know their specific roles, and trust each other. This helps turn a hectic situation into calm and organized.
- Parents and caregivers are often present during pediatric arrests. Including them with empathy, while maintaining focus on the child, can help support them emotionally and even help in medical history or decision-making when seconds matter.
Step-by-Step Breakdown Of Algorithm
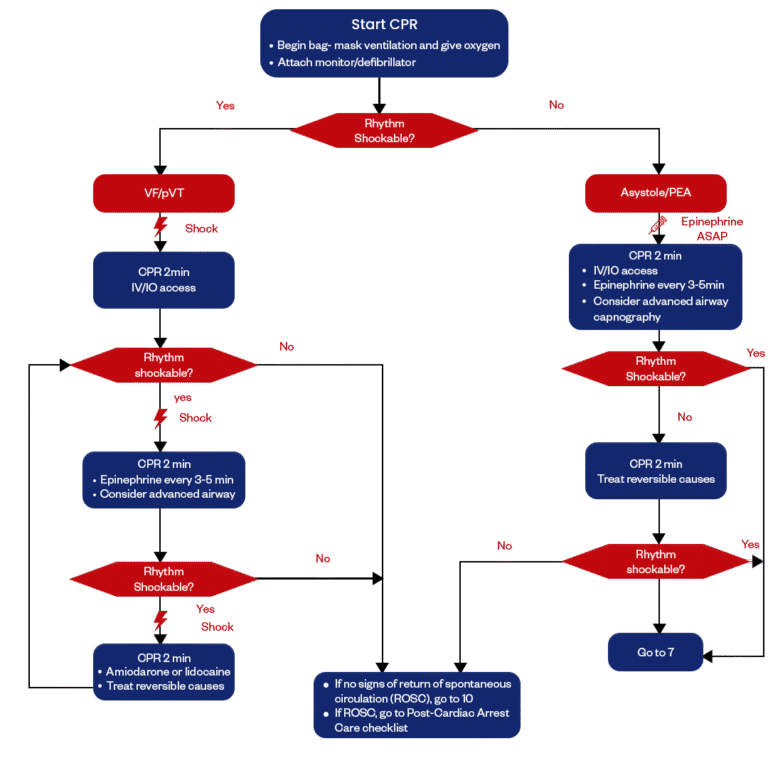
Let’s break down this algorithm step by step, so it will guide you through each part in a simple way.
01.
Start CPR
The very first thing you do is begin high-quality CPR right away. At the same time, you start bag-mask ventilation and provide oxygen to help oxygenate the blood. It’s also important to attach the monitor or defibrillator as soon as possible. Once everything’s in place, you check the rhythm. If it turns out to be shockable, like VF or pVT, you move on to Step 2. If it’s not shocking, you skip ahead to Step 9.
02.
Assess Rhythm — Is it VF or pVT?
Now that the monitor is on, you take a closer look at the rhythm. If it’s Ventricular Fibrillation (VF ) or Pulseless Ventricular Tachycardia (pVT), you know you’re dealing with a shockable rhythm. In that case, it’s time to move to Step 3. If it’s something else, you’ll handle it differently later.
03.
Deliver The First Shock
As soon as you confirm a shockable rhythm, you deliver a shock right away. This electrical therapy is critical; it gives the heart a chance to reset and hopefully return to a normal rhythm.
04.
Resume CPR for 2 minutes.
After the shock, you go right back into CPR without delay. During these two minutes, you work on getting IV (Intravenous ) or IO (Intraosseous ) access so you're ready to administer medications. At the end of the cycle, you reassess the rhythm to determine if another shock is needed. If it is, you continue to Step 5. If it’s no longer shocking, you jump to Step 12.
05.
Reassess rhythm and deliver another shock if indicated
You take another look at the rhythm. If VF or pVT persists, you deliver another shock. It's all about giving the heart another chance to react while you keep up good chest compressions in between.
06.
Continue CPR and Administer Epinephrine
CPR continues for another 2 minute cycle. During this time, you administer epinephrine every 3 to 5 minutes to help stimulate the heart. You also consider placing an advanced airway and using capnography to check the effectiveness of compressions and ventilation. After this cycle, you check the rhythm again to see if it’s shockable, and you head to Step 7. If not, you go back to Step 12.
07.
Deliver a Third Shock if Rhythm Persists
If the rhythm remains shockable, you deliver another shock. These repeated shocks are vital for improving the chance of defibrillation success. You keep going with the algorithm to stay ahead of the arrest.
08.
Continue CPR, Give Antiarrhythmics, and Treat Causes
After the third shock, you immediately resume CPR for another 2 minutes. This time, you consider giving antiarrhythmic medicines like amiodarone or lidocaine. It's also crucial to evaluate for and treat any reversible causes, like hypoxia or tension pneumothorax. Once that’s done, you reassess the rhythm again if it’s still shockable, you go back to Step 5. If not, you continue to Step 12.
09.
For Asystole or PEA, Administer Epinephrine Immediately
If the rhythm is not shockable and shows asystole or PEA(Pulseless Electrical Activity ), you act fast by giving epinephrine right away. These rhythms don’t respond to shocks, so medication and continuous CPR are your best tools.
10.
Continue CPR and Secure IV/IO Access
CPR continues for another 2 minutes. During this time, you make sure you’ve established IV or IO access and keep giving epinephrine every 3 to 5 minutes. You also evaluate whether to insert an advanced airway and use capnography to monitor effectiveness. At the end of the cycle, you check the rhythm again—if it turns shockable, you go to Step 7. If not, you move to Step 11.
11.
Keep CPR Going and Reassess for Reversible Causes
You continue CPR for yet another 2 minutes cycle and take a closer look at any reversible causes that may be contributing to the arrest. At the end of this cycle, you reassess the rhythm again. If it becomes shocking, you go back to Step 7. If it remains non-shockable, you move to Step 12.
12.
ROSC or Continue Resuscitation
Has the patient achieved Return of Spontaneous Circulation (ROSC)? If yes, you immediately begin post-cardiac arrest care. If not, you continue CPR and look back to Step 10 to repeat the cycle. This point is all about deciding whether to persist or shift your focus based on the patient’s response.
Sidebar for the Pediatric Cardiac Arrest Algorithm
I. CPR Quality
- Push hard (at least one-third of the anteroposterior diameter of the chest) and fast (100 to 120 per minute), and allow complete chest recoil.
- Minimize interruptions in compressions.
- Change the compressor every 2 minutes, or sooner if fatigued.
- If no advanced airway, 15:2 compression to ventilation ratio.
- If an advanced airway is used, provide continuous compressions and give a breath every 2 to 3 seconds.
II. Shock Energy for Defibrillation
- First shock: 2 Joules per kilogram.
- Second shock: 4 Joules per kilogram.
- Subsequent shocks: At least 4 Joules per kilogram, up to a maximum of 10 Joules per kilogram or adult dose.
III. Drug Therapy
- Epinephrine IV or IO dose: 0.01 milligrams per kilogram (0.1 milliliter per kilogram of the 0.1 milligram per milliliter concentration). Maximum dose: 1 milligram. Repeat every 3 to 5 minutes. If no IV or IO access, may give endotracheal dose of 0.1 milligrams per kilogram (0.1 milliliter per kilogram of the 1 milligram per milliliter concentration).
- Amiodarone IV or IO dose: 5 milligrams per kilogram bolus during cardiac arrest. May repeat up to 3 total doses for
- Lidocaine IV or IO dose: Initial: 1 milligram per kilogram loading dose.
IV. Advanced Airway
- Endotracheal intubation or supraglottic advanced airway.
- Waveform capnography or capnometry to confirm and monitor ET tube placement.
V. Reversible Causes
- H: Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hypoglycemia Hypokalemia or hyperkalemia, Hypothermia
- T: Tension pneumothorax, Tamponade, cardiac, Toxins, Thrombosis (pulmonary), Thrombosis (coronary)
Synopsis of Pediatric Cardiac Arrest Algorithm
The Pediatric Cardiac Arrest Algorithm offers a structured approach for healthcare providers to respond effectively when a child experiences cardiac arrest. In these critical moments, it’s crucial to first ensure the scene is safe, call for help, and begin high-quality CPR. The algorithm emphasizes the importance of quick assessment, securing an airway, and delivering appropriate interventions based on the child’s age and underlying conditions. Whether your role is in a hospital, clinic, or community setting, understanding this algorithm can significantly improve outcomes. At Bayside CPR, we’re dedicated to equipping you with the skills and knowledge necessary to act confidently in emergencies. Ready to enhance your lifesaving abilities? Join us for our training session!
Frequently Asked Questions
What should I do if I'm unsure whether a child is in cardiac arrest?
- If you’re unsure whether a child is in cardiac arrest, check for responsiveness and normal breathing; if they’re unresponsive and not breathing normally, start CPR and call 911 for help immediately. It’s always better to act quickly, even if you’re uncertain.
Does the age of the child affect how I assess cardiac arrest?
- Yes, the age of the child impacts your assessment since infants and younger children may present differently than older kids, especially in how you check for responsiveness and pulse. Always remember that younger kids can often have hidden heart conditions, so stay alert to any signs of distress.
What distinguishes pediatric cardiac arrest from adult cardiac arrest?
- Pediatric cardiac arrest usually results from respiratory cases or trauma, while adults typically experience it from heart disease; this difference affects how you approach the situation. Understanding these distinctions helps you respond more effectively.
What are the doses for the pediatric cardiac arrest algorithm?
- For the pediatric cardiac arrest algorithm, the standard doses include 0.01 mg/kg of epinephrine for IV/IO administration every 3–5 minutes, with a maximum of 1 mg per dose, and you should also consider the right dosage for any medication based on their weight.
How can I prepare myself for recognizing and responding to pediatric cardiac arrest?
- To prepare for recognizing and responding to pediatric cardiac arrest, consider taking a CPR and first aid class that focuses on children; practicing these skills can boost your confidence when faced with an emergency. Additionally, staying familiar with pediatric emergency procedures and resources can make a huge difference in critical moments.