
PALS Tachycardia Algorithm for Pediatric Patients
When a child’s heart starts racing faster than it should, it can be a real emergency, and knowing what to do in those critical moments can make all the difference. Tachycardia simply means a faster-than-normal heart rate, also known as accelerated cardiac activity. But in pediatric patients, what’s considered “too fast” depends on the child’s age.
For example, what’s normal for a newborn is much faster than for a teenager, which is why the PALS Algorithm Tachycardia is so crucial. It provides the pediatric care team with a clear, step-by-step guide to manage these emergencies quickly and effectively, helping everyone from nurses to paramedics work together seamlessly when every second counts. When assessing a child with tachycardia in Pediatric Advanced Life Support, as a healthcare providers, you should focus on vital signs like heart rate, blood pressure, respiratory rate, and oxygen saturation, along with signs of poor perfusion such as skin color and temperature. Also, look for indicators of instability like hypotension, altered mental status, and shock, which suggest that the tachycardia might be affecting the child’s circulation.
In this guide, we’ll break down what tachycardia means for kids, review normal heart rate ranges by age, and explain how the PALS Tachycardia Algorithm helps save lives when a child’s heart needs urgent help. Additionally, read The PALS secondary assessment, which helps identify the underlying cause of the tachycardia, which then informs the appropriate application of the PALS tachycardia algorithm.

Normal Heart Rate Vs. Heart Rate In Tachycardia
Curious about how a child’s normal heart rate compares to the faster heartbeat seen in tachycardia? Let’s explore what these differences mean for kids’ health and well-being.
Age Group | Normal Heart Rate (bpm) | Tachycardia (bpm) |
Infants (1-12 Months) | 80-160 bpm | 160+ bpm |
Toddlers (1-2 Years) | 80-130 bpm | 130+ bpm |
Preschool (3-5 Years) | 80-120 bpm | 120+ bpm |
School Age ( 6-11+ Years) | 70-120 bpm | 120+ bpm |
Types Of PALS Tachycardia
1. Supraventricular Tachycardia (SVT) :
- Supraventricular tachycardia (SVT) is a rapid heart rate above the ventricles, often over 200 bpm in infants or 180 bpm in children, caused by reentrant circuits or abnormal pathways. Symptoms include a racing heart, dizziness, and shortness of breath. It can be managed with observation, medications, vagal maneuvers, or procedures like ablation. According to Science Direct, supraventricular tachycardia (ST) affects 1 in 500 children.
2. Sinus Tachycardia ( ST) :
- Sinus tachycardia is a normal, increased heart rate due to higher physiological demand, originating from the sinus node. In infants, it's over 160-170 bpm; in children aged 3-11, over 120 bpm. Causes include fever, activity, stress, or conditions like infections, hyperthyroidism, and anemia. Symptoms include dizziness and palpitations. Treatment varies based on heart rate, often involving beta-blockers or calcium channel blockers.
3. Ventricular Tachycardia (VT) :
- Ventricular tachycardia (VT) is a rapid heartbeat originating from the ventricles, often over 100 bpm in children, sometimes exceeding 200 bpm. It can be caused by heart disease, structural issues, or prior surgery. Symptoms include dizziness, chest pain, fainting, or cardiac arrest. Therapy options include medication, cardioversion, ablation, ICD (implantable cardioverter-defibrillator), surgery, or pacemakers.
Common Causes of Tachycardia In Children
Tachycardia in children can be caused by a variety of reasons, from common factors like fever and dehydration to more complex issues like structural heart problems or cardiac arrhythmias. It is crucial to identify it quickly to save the life of a pediatric patient.
Category | Examples |
Physiological | Fever, anxiety, dehydration, or pain |
Structural Heart Disease | Congenital heart defects or cardiomyopathies |
Infections | Myocarditis, sepsis, or other systemic infections |
Electrolyte Imbalances | Hypokalemia, hypomagnesemia |
Medications and Toxins | Stimulants, caffeine, or certain drugs |
Autonomic Nervous System Factors | Stress or sympathetic stimulation |
Step-By-Step Breakdown Of PALS Tachycardia Algorithm With Pulse
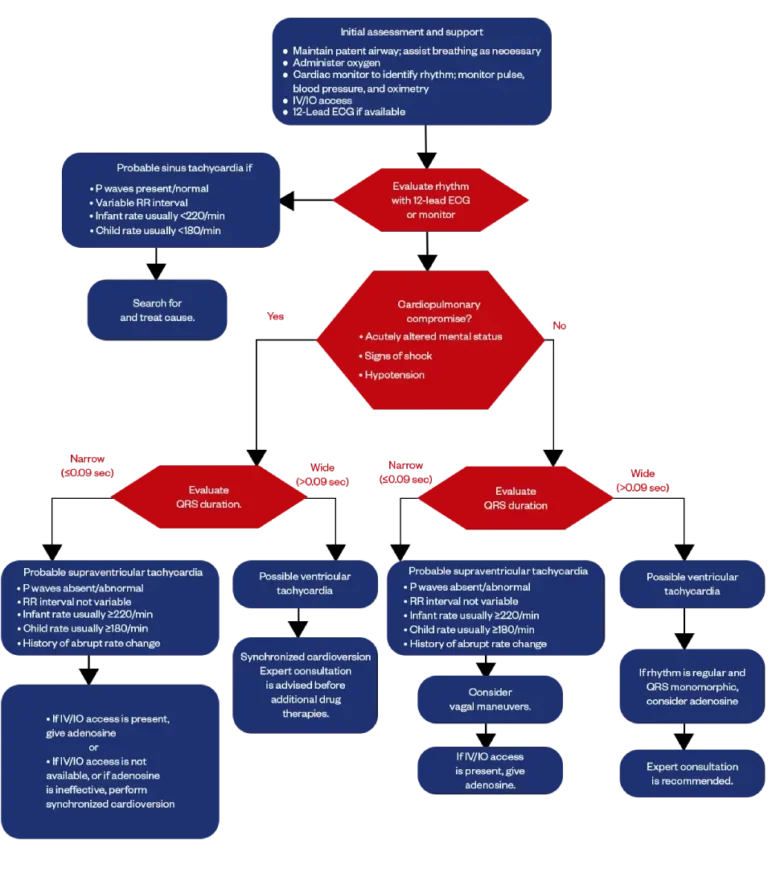
Dealing with tachycardia with a pulse can be tough, but understanding the PALS tachycardia protocol makes it more manageable. Let’s walk through the steps together so you understand what to do when every second counts.
01.
Initial assessment and support
The first step in managing a pediatric tachycardia is rapid assessment and stabilization. Ensure a clear airway, assist breathing if needed, and administer oxygen. Connect the patient to a cardiac monitor to identify the rhythm, and monitor pulse, blood pressure, and oxygen levels closely. Establish IV or IO access early for medication or fluid administration. If available, obtain a 12-lead ECG to better evaluate the heart’s activity.
02.
Evaluate rhythm with a 12-lead ECG or monitor
Once the initial support is in place, the next step is to evaluate the pediatric heart rhythm using a monitor or a 12-lead ECG if you have one available. Take a close look at the rhythm. If it appears to be probable sinus tachycardia, you’ll move on to Step 3 for further evaluation and management. However, if the rhythm suggests that the pediatric patient is experiencing signs of cardiopulmonary compromise, it’s critical to skip ahead and go directly to Step 5, where more advanced interventions are needed.
03.
Probable sinus tachycardia if
You're looking for signs that the rhythm is consistent with probable sinus tachycardia. For a pediatric patient, that means the P waves should be present and appear normal, and the R-R intervals can vary. In terms of heart rate, an infant typically has a rate less than 220 bpm, while a child usually has a rate under 180 bpm. If all these findings line up, you can move on to Step 4 for further assessment and care.
04.
Search for and treat the cause
Your focus shifts to finding out what’s causing the tachycardia and addressing it directly. In pediatric cases, common causes can include pain, hypoxia, fever, dehydration, or anxiety. Take a good look at the overall clinical picture, check for signs of infection, evaluate the fluid level, ensure the child is getting enough oxygen, and manage any discomfort or stress. The goal here is to treat the underlying issue rather than the heart rate itself, since tachycardia is usually a response to something else going on in the body.
05.
Is there cardiopulmonary compromise?
It's time to determine whether the patient is showing signs of cardiopulmonary compromise. Look for key indicators like an acutely altered mental status, signs of shock (such as cool extremities, delayed capillary refill, or weak pulses), and hypotension. These signs suggest that the heart isn't effectively supporting circulation. If any of these red flags are present, move immediately to Step 6 for urgent intervention. If none are present, and the child appears more stable, you can skip ahead to Step 11 for continued evaluation and care.
06.
Evaluate QRS duration
It's all about evaluating the QRS duration on the ECG (electrocardiogram) to help narrow down the type of tachycardia you're dealing with. Take a close look at the width of the QRS complex. If it’s narrow, meaning 0.09 seconds or less, then you’ll move on to Step 7, which focuses on managing narrow-complex tachycardia. However, if the QRS is wide, greater than 0.09 seconds, that points to a different mechanism, and you should skip ahead to Step 9 for appropriate treatment of wide-complex tachycardia.
07.
Probable supraventricular tachycardia
You're assessing for probable supraventricular tachycardia (SVT), especially in the context of a narrow QRS complex. Key signs to look for include absent or abnormal P waves and an RR interval that stays consistent, rather than varying. In terms of heart rate, an infant generally has a rate of 220 bpm or higher, while a child usually presents with a rate of 180 bpm or higher. A helpful clue is a history of sudden onset; SVT often starts and stops abruptly. If all these signs point to SVT, go ahead and move on to Step 8 for management.
08.
IV/IO Access and Adenosine
The next action is to establish IV/IO access if you haven’t already. If access is available, you’ll administer adenosine to help break the supraventricular tachycardia. Adenosine works by temporarily blocking the electrical signals in the heart, which can reset the rhythm. However, if IV/IO access isn’t available or if adenosine doesn’t work to restore normal rhythm, the next step is to perform synchronized cardioversion. This procedure involves delivering a controlled shock to the heart to reset its rhythm and bring it back to normal.
09.
Possible ventricular tachycardia
You’re considering the possibility of ventricular tachycardia (VT), which generally presents with a wide QRS complex. If you suspect VT, it's crucial to move quickly to Step 10 for further evaluation and treatment, as this rhythm can be life-threatening and requires immediate intervention.
10.
Synchronized cardioversion
If ventricular tachycardia (VT) is confirmed or highly suspected, synchronized cardioversion is the next step to restore normal rhythm. This procedure involves delivering a steady shock to the heart while it’s in the right phase of the cardiac cycle. It’s important to consult with an expert before considering additional drug therapies, as VT is a serious condition, and further treatments need to be tailored to the specific situation based on expert guidance.
11.
Evaluate QRS duration
You need to evaluate the QRS duration once again. If the QRS complex is narrow (0.09 seconds or less), you’ll proceed to Step 12 for further management of the tachycardia. On the other hand, if the QRS is wide (greater than 0.09 seconds), it’s time to skip ahead to Step 15 for a different approach to treatment.
12.
Probable supraventricular tachycardia
You’re once again assessing for probable supraventricular tachycardia (SVT), particularly with a narrow QRS complex. Look for signs like absent or abnormal P waves, and a consistent RR interval (not varying). In infants, the heart rate is usually 220 bpm or higher, while in children, it’s typically 180 bpm or more. A key clue is a history of a sudden onset or abrupt rate change, which is common with SVT. If these signs point to SVT, proceed to Step 13 for further management.
13.
Consider vagal maneuvers
You should consider using vagal maneuvers as an initial, non-invasive way to treat supraventricular tachycardia (SVT) in a stable pediatric patient. These techniques, such as an ice pack to the face for infants or having an older child blow through a straw, can stimulate the vagus nerve and help slow down the heart rate. If the vagal maneuvers are ineffective or not appropriate, you'll move on to Step 14 for the next line of treatment.
14.
If IV/IO access is present, give adenosine
If IV/IO access is available, administer adenosine to treat the suspected supraventricular tachycardia. Adenosine works by briefly blocking conduction through the AV node, which can interrupt the abnormal rhythm and restore normal sinus rhythm. It’s most effective when given as a rapid IV push, followed instantly by a flush. Be sure to observe the patient closely during and after administration.
15.
Possible ventricular tachycardia
It is based on the presence of a wide QRS complex, you're now considering possible ventricular tachycardia (VT). This rhythm can be serious, even if the patient seems stable, so it’s important to act quickly. Move ahead to Step 16 for evaluation and proper management.
16.
If the rhythm is regular and QRS monomorphic, consider adenosine
You should consider using vagal maneuvers as an initial, non-invasive way to treat supraventricular tachycardia (SVT) in a stable pediatric patient. These techniques, such as an ice pack to the face for infants or having an older child blow through a straw, can stimulate the vagus nerve and help slow down the heart rate. If the vagal maneuvers are ineffective or not appropriate, you'll move on to Step 14 for the next line of treatment.
17.
Expert consultation is recommended
It’s time to bring in additional support, expert consultation is strongly recommended. Ventricular tachycardia, especially when continuous or unclear in origin, can be difficult to manage and need advanced interventions or individualized therapies. Consulting a pediatric cardiologist or other capable specialist ensures the patient receives the safest and most effective care moving forward.
Sidebar Of Algorithm
1. Doses and Details
Synchronized cardioversion
- Begin with 0.5-1 J/kg; if not effective, increase to 2 J/kg. Sedate if needed, but don’t delay cardioversion.
2. Drug Therapy
Adenosine IV/IO dose
- First dose: 0.1 mg/kg rapid bolus (maximum:6 mg)
- Second dose: 0.2 mg/kg rapid bolus(maximum second dose: 12 mg)
Final Thoughts on Implementing the PALS Tachycardia Algorithm
In short, the PALS Algorithm for tachycardia depends on staying calm, thinking critically, and acting swiftly. Recognize early signs, including changes in mental status, perform further assessment as needed, and seek expert consultation when necessary to ensure the best care. Immediate treatment is essential, whether managing narrow or wide complex tachycardia. Regular practice and a solid understanding of the concepts help you act confidently in high-pressure moments. Remember, the flowchart is a tool to guide safe, timely, and life-saving care. Ready to improve your skills? Enroll in a PALS certification course with Bayside CPR and boost your confidence in emergencies!
Frequently Asked Questions
What is the primary treatment approach for unstable tachycardia in pediatric patients?
- Immediate synchronized cardioversion is the primary treatment for unstable tachycardia in pediatric patients. This approach restores a normal heart rhythm when the patient is experiencing signs of hemodynamic compromise or shock.
How to manage tachycardia in pediatrics?
- Managing pediatric tachycardia relies on the type (narrow vs. wide complex), stability, underlying cause, and age of the child.
How do I differentiate between sinus and supraventricular tachycardia (SVT) in children?
- Differentiating between ST and SVT in children can be done by considering factors like heart rate, the presence and appearance of P-waves on an ECG, and the onset of the fast heart rate.
- Infant: ST is usually < 220 bpm; SVT is usually > 220 bpm
Child: ST is usually < 180 bpm; SVT is usually > 180 bpm
When should I take my child to the Emergency Room for tachycardia?
- You should take your child to the ER for tachycardia if your child has symptoms such as a racing heart, dizziness, chest pain, or fainting, and it is hard to wake up.
What causes a child's heart to beat fast?
- There are a large number of reasons for the heart to beat faster than expected, from simple physiological causes, such as excitement or physical activity, to illness, such as a fever, and a range of diseases of the heart or metabolism.


