When a medical emergency like Sudden Cardiac Arrest(SCA) occurs, where the heart suddenly stops beating effectively, leading to loss of blood flow to the brain and other vital organs, immediate response is everything. According to the American Heart Association (AHA), over 350,000 out-of-hospital cardiac arrests occur each year in the United States alone, with survival rates below 10%. One of the main reasons for not being able to save a cardiac arrest patient is that we miss a critical step of treating the reversible causes right away. These are things like low oxygen, blood loss, or blocked arteries, which we must identify and treat early.
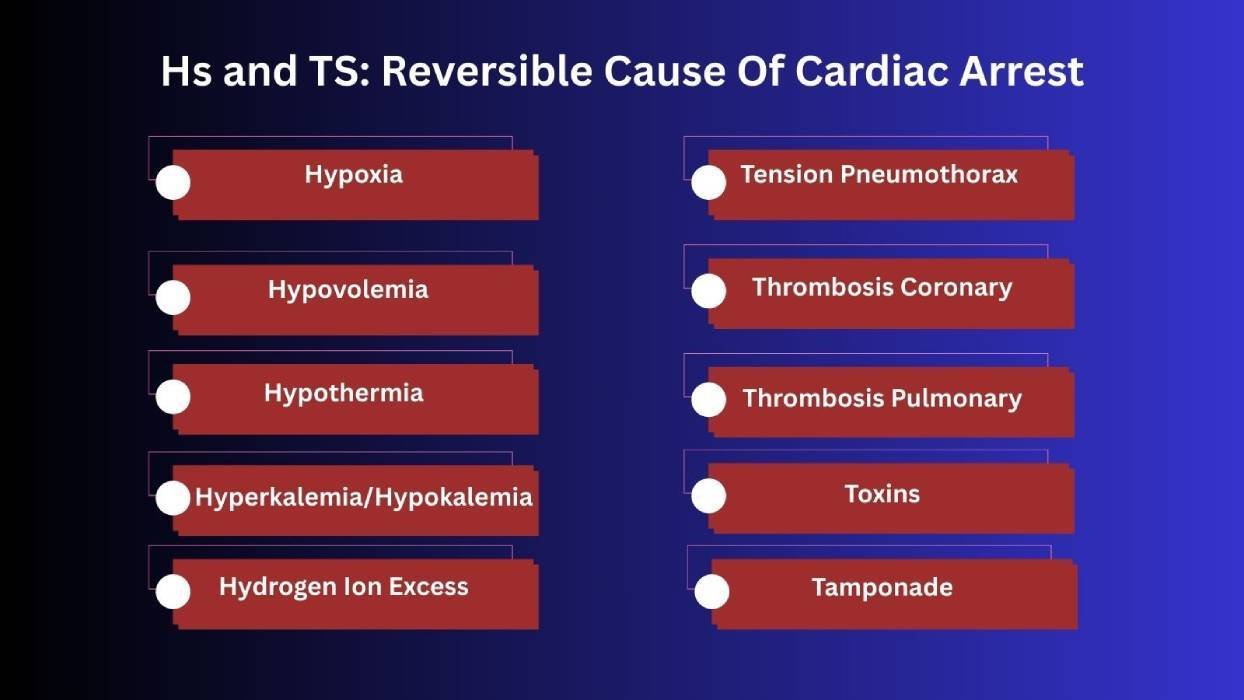
The 5 Hs and Ts of Cardiac Arrest
Hs and Ts of ACLS are the terms that refer to the 10 reversible causes of Cardiac arrest; 5 of each, that we need to assess immediately and treat during Cardiopulmonary resuscitation (CPR) or advanced cardiac life support (ACLS). The “Hs” include conditions like low blood volume and oxygen, while “Ts” cover life-threatening issues like toxins and clots. Read through this guide to learn how to identify each H and T, understand their dangers, and know the right actions to take in an emergency.
5 H’s: Reversible Causes of Cardiac Arrest
In emergency situations, identifying and managing issues quickly can make the difference between life and death. The Hs include the causes like low oxygen, blood loss, or chemical imbalances. Let’s break down each one so you know how to recognize and respond to them.
1. Hypovolemia (Low Blood Volume)
Hypovolemia is one of the most common and treatable causes of cardiac arrest, which happens when the body loses too much blood or fluid, making it hard for the heart to pump effectively. This leads to decreased blood volume, which can reduce oxygen delivery to vital organs. When oxygen levels stay low for too long, it can result in low blood pressure, a slow heart rate (bradycardia), and, if not addressed quickly, sudden cardiac arrest.
Causes:
- Trauma: Injuries like accidents or severe wounds can cause significant blood loss.
- Hemorrhage (Severe Bleeding): Uncontrolled internal or external bleeding rapidly reduces circulating blood volume and can quickly lead to hypovolemic cardiac arrest.
- Dehydration: When the body loses more fluids than it takes in, often due to vomiting, diarrhea, or inadequate fluid intake.
- Internal Bleeding: Bleeding inside the body, such as from a ruptured organ or blood vessel, reduces blood volume.
- Severe Burns: Damage to the skin and blood vessels causes fluid loss, leading to a drop in blood volume.
Symptoms:
- Rapid heart rate (tachycardia)
- Narrow QRS complex on ECG
- Weak or absent pulse
- Pale Skin
- Low blood pressure
- Visible bleeding or signs of fluid loss
Treatment:
- Secure IV or IO access
- Rapid infusion of fluids (normal saline or Ringer’s lactate)
- Control any bleeding
- Consider a blood transfusion if blood loss is severe
2. Hypoxia (Lack of Oxygen)
Hypoxia (Lack of Oxygen) occurs when the body or brain doesn’t get enough oxygen to function properly. It’s a critical and reversible cause of cardiac arrest resulting from blocked airways, lung problems, or poor ventilation. If we do not treat it immediately, it leads to low blood pressure, a slow heart rate, and then cardiac arrest.
Causes:
- Blocked Airway: Obstructions like choking prevent air from reaching the lungs.
- Respiratory Failure: The lungs fail to efficiently exchange gases, reducing oxygen levels.
- Low Oxygen Environment: Areas with insufficient oxygen, like high altitudes or confined spaces, limit oxygen intake.
Symptoms:
- Cyanosis (blue lips or fingertips)
- Minimal or absent chest movement during ventilation
- Low oxygen saturation (SpO₂)
- Confusion or loss of consciousness
Treatment:
- Ensure the airway is open and clear
- Provide high-flow oxygen
- Use bag-mask ventilation if needed
- Intubation and mechanical ventilation if necessary
3. Hydrogen Ion Excess (Acidosis)
Causes:
- Respiratory Failure: When the lungs can’t remove enough carbon dioxide, it builds up in the blood and forms acid.
- Sepsis: A severe infection can cause widespread inflammation, leading to acid accumulation in the bloodstream.
- Kidney Failure: The kidneys are responsible for removing excess acid; when they fail, acid levels in the blood rise.
Symptoms:
- Deep, fast breathing (in metabolic acidosis)
- ECG changes
- Low pH on arterial blood gas (ABG)
- Decreased responsiveness
Treatment:
- Provide effective ventilation (for respiratory acidosis)
- ECG changes
- Administer sodium bicarbonate (for metabolic acidosis, especially if severe or with known overdose)
- Treat the underlying cause like sepsis, shock
4. Hyperkalemia or Hypokalemia (Too Much or Too Little Potassium)
Hyperkalemia or Hypokalemia refers to having too much or too little potassium in the blood, and both are very dangerous conditions that lead to cardiac arrest. Potassium plays a key role in maintaining normal heart rhythm, so any imbalance can disrupt electrical signals in the heart. High potassium (hyperkalemia) can cause the heart to beat irregularly or stop, while low potassium (hypokalemia) can weaken heart function and lead to arrhythmias. These imbalances are often found in patients with kidney problems, medication side effects, or dehydration, and must be treated quickly to stabilize heart rhythm and prevent cardiac arrest.
Hyperkalemia (High Potassium)
Causes:
- Kidney Failure: The kidneys normally remove excess potassium, so when they fail, potassium builds up in the blood.
- Medications: Certain drugs, like potassium-sparing diuretics or ACE inhibitors, can raise potassium levels.
- Acidosis: Increased acidity in the blood causes potassium to shift from inside the cells into the bloodstream.
- Tissue Breakdown: Severe injury, burns, or conditions like rhabdomyolysis can release large amounts of potassium from damaged cells.
Symptoms:
- Peaked T-waves on ECG
- Widened QRS complex
- Muscle weakness or paralysis)
- Cardiac arrhythmias
Treatment:
- IV calcium chloride or gluconate (stabilizes the heart)
- IV insulin + glucose (shifts potassium into cells)
- Sodium bicarbonate (if acidotic)
- Albuterol (inhaled)
- Dialysis or sodium polystyrene sulfonate (Kayexalate) for removal
Hypokalemia (Low Potassium)
Causes:
- Diuretics: These medications increase urine output, which can lead to excessive potassium loss.
- Vomiting: Frequent vomiting causes the body to lose both fluids and essential electrolytes like potassium.
- Diarrhea: Similar to vomiting, prolonged diarrhea can deplete potassium levels through fluid loss.
- Poor Intake: Not getting enough potassium through diet, especially during illness or malnutrition, can lead to deficiency.
Symptoms:
- Flattened T-waves, U-waves, or prolonged QT on ECG
- Muscle weakness or cramps
- Risk of arrhythmias
Treatment:
- Careful IV potassium replacement
- Oral potassium supplements (if non-emergent)
- Avoid rapid undiluted IV potassium (can be dangerous)
5. Hypothermia (Low Body Temperature)
Hypothermia is a reversible cause of cardiac arrest that occurs when the body’s core temperature drops too low, usually below 35°C (95°F). Cold temperatures can slow down the heart, reduce breathing and circulation, and make the body less responsive to medications and defibrillation. In severe cases, hypothermia can lead to loss of consciousness and cardiac arrest.
Causes:
- Cold Exposure: Prolonged exposure to cold weather or water can cause the body’s temperature to drop dangerously low.
- Trauma Victims: Injured individuals may be more vulnerable to hypothermia, especially if they are exposed to the elements or experience significant blood loss.
- Drowning: Cold water immersion lowers body temperature rapidly, especially if rescue is delayed.
Symptoms:
- Body temperature below 35°C (95°F)
- Cold, pale skin
- Bradycardia (slow heart rate)
- Decreased responsiveness or coma
Treatment:
- Warm the patient with blankets, warm IV fluids, and heated oxygen
- Cold, pale skin
- Continue CPR during rewarming
- Medications and defibrillation may not work until the core temp is above 30°C (86°F)
5 T’s: Reversible Causes of Cardiac Arrest
The T reversible causes of reversible cardiac arrest focus on physical problems that block or disrupt the heart’s function. These include trauma, pressure buildup, and clots. Here’s a breakdown to help you recognize and respond to each one:
1. Tension Pneumothorax
Tension Pneumothorax is a reversible cause of cardiac arrest that occurs when air becomes trapped in the space between the lung and chest wall. This trapped air puts pressure on the lungs and heart, making it hard to breathe and stopping blood from circulating properly. It can quickly lead to collapse of the affected lung, low blood pressure, and cardiac arrest if not treated immediately.
Causes:
- Chest Trauma: A penetrating or blunt injury can cause air to leak into the space around the lungs (pleural space), trapping it under pressure.
- Lung Injury: Conditions like a ruptured lung or complications from mechanical ventilation can also allow air to escape into the pleural space.
Symptoms:
- Sudden shortness of breath
- Tracheal deviation (late sign)
- Uneven chest movement and breath sounds
- Jugular vein distension (JVD)
- No pulse during CPR
Treatment:
- Immediate needle decompression (2nd intercostal space, midclavicular line) followed by chest tube insertion
2. Tamponade (Cardiac)
Cardiac Tamponade is a condition where fluid builds up around the heart in the pericardial sac, putting pressure on the heart and preventing it from pumping effectively. This pressure reduces blood flow to the body and can quickly lead to shock or cardiac arrest. It can be caused by trauma, cancer, infections, or medical procedures. Early signs can be subtle, so quick diagnosis and emergency treatment, like pericardiocentesis (draining the fluid) are crucial for survival.
Causes:
- Trauma: Chest injuries, especially penetrating wounds, can cause blood to leak into the pericardial sac, putting pressure on the heart.
- Cancer: Some cancers can lead to fluid buildup around the heart, either from tumor spread or as a complication of treatment.
- Infection: Infections like pericarditis can cause inflammation and fluid accumulation in the sac surrounding the heart.
Symptoms:
- Narrow QRS, rapid heart rate
- Muffled heart sounds
- Jugular vein distension
- No pulse or hard to feel pulse
- Pulsus paradoxus (BP drops during inhalation)
Treatment:
- Pericardiocentesis: emergency needle drainage of the fluid, monitoring with ultrasound if available
3. Toxins (Drug Overdose or Poisoning)
Toxins that includes drug overdoses or chemical poisoning, are a reversible cause of cardiac arrest that can severely disrupt the heart’s rhythm and function. Substances like tricyclic antidepressants, beta-blockers, calcium channel blockers, or street drugs like cocaine slow the heart, affect breathing, or cause seizures and unconsciousness. On-time identification, supportive care, and use of specific antidotes or poison control guidance are essential to reverse the effects and save the patient’s life.
Causes:
- Prescription Medications: Overdoses of drugs like tricyclic antidepressants, digoxin, beta-blockers, or calcium channel blockers can interfere with the heart’s electrical activity and muscle function.
- Recreational Drugs: Substances such as cocaine or opioids can cause dangerous heart rhythms, respiratory depression, or cardiac arrest.
- Poisoning: Ingesting or being exposed to toxic substances, intentionally or accidentally, can affect heart rate, blood pressure, and overall cardiac stability.
Symptoms:
- ECG changes (e.g., prolonged QT, bradycardia)
- Dilated or pinpoint pupils
- Seizures, confusion, coma
- No pulse or weak circulation
Treatment:
- Support airway and circulation
- Use specific antidotes like naloxone for opioids, calcium for calcium channel blockers
- Contact poison control
- If airway is protected and feel appropriate to use, activate charcoal
4. Thrombosis – Coronary (Heart Attack)
Coronary Thrombosis is a blockage in one of the heart’s arteries, usually caused by a blood clot, and is a major reversible cause of cardiac arrest. This blockage prevents oxygen-rich blood from reaching heart muscle, leading to a heart attack (myocardial infarction). If not treated quickly, the affected part of the heart can stop working, which may lead to sudden cardiac arrest.
Causes:
- Coronary Artery Blockage: A blood clot can form in a coronary artery, which supplies blood to the heart muscle.
- Myocardial Infarction (MI): When the artery is blocked, part of the heart muscle is starved of oxygen, leading to a heart attack.
Symptoms:
- Chest pain before arrest
- ECG: ST-elevation, Q-waves, or T-wave inversions
- Elevated cardiac enzymes
Treatment:
- If the blockage is identified before cardiac arrest, it’s treated with procedures like angioplasty (PCI) to open the artery or clot-busting medications (fibrinolytics) to dissolve the clot.
- If the patient is already in cardiac arrest, CPR should be continued, but using fibrinolytics during CPR is not usually recommended unless a pulmonary embolism (PE) is strongly suspected.
5. Thrombosis – Pulmonary (Pulmonary Embolism)
Pulmonary Thrombosis, also known as Pulmonary Embolism, occurs when a blood clot travels to the lungs, blocking the main artery and preventing blood flow. This can cause sudden shortness of breath, chest pain, and in severe cases, cardiac arrest.
Causes:
- Blood Clot Formation: A clot, usually from a deep vein in the leg (DVT), can travel to the lungs.
- Blocked Pulmonary Artery: The clot lodges in a pulmonary artery, blocking blood flow to part of the lung.
Symptoms:
- Sudden collapse, no pulse
- Rapid heart rate
- History of DVT, recent surgery, or prolonged immobility
- Positive D-dimer or imaging (if done earlier)
Treatment:
- Fibrinolytic therapy (clot-busting drugs)
- Surgical embolectomy (if available)
- Continue CPR until treatment can be given
Final Thoughts: H’s and T’s of Cardiac Arrest
The Hs and Ts represent a crucial framework for identifying reversible causes of cardiac arrest. By focusing on the above-mentioned specific causes, i.e, 5Hs and 5Ts, healthcare providers assess and treat the underlying conditions. Early recognition and prompt intervention of these reversible causes significantly improve the chances of survival and recovery for patients suffering cardiac arrest. With cardiac arrest, there’s no time to waste.
Build the confidence to act in emergencies with Bayside CPR. Our flexible certification programs are created for busy professionals, letting you complete the online coursework on your own schedule before attending a quick 30-minute, in-person skills session at one of our 60+ locations. You’ll earn your AHA Standard ACLS, BLS, PALS, CPR, or First Aid certification and receive your card the same day.