Understanding ECG | EKG (Electrocardiogram) rhythms is a crucial part of ACLS, it can be the difference between life and death of a cardiac arrest patient . Recognizing and analyzing these practices quickly helps health providers and doctors to respond effectively in emergencies. In this overview, we’ll explore why mastering electrocardiography interpretation is so important and walk through the key skills needed to read these rhythms confidently during ACLS situations. Whether you’re getting ready for your ACLS certification or just reviewing your skills, this guide highlights the key rhythms you must identify to deliver quick, evidence-based care during emergencies. Let’s get started!
The Prototypical ECG Tracing
The prototypical electrocardiogram tracing is a standardized representation of the electrical activity of the heart. It helps medical professionals assess heart rhythm, conduction irregularities, ischemia, infarction, electrolyte imbalances, and more.
- The P wave represents the movement of an electrical signal through the atria, indicating atrial depolarization, which typically leads to atrial contraction.
- The QRS complex reflects the electrical depolarization of both the left and right ventricles and is generally associated with ventricular contraction.
- The T wave represents the repolarization phase of the ventricles, when they recover electrically after contraction.
If you’re new to reading ECGs or want a refresher, check out our guide on PQRST wave: A guide to ECG interpretation, it breaks down the key components of the ECG in a simple, approachable way.
Importance of Understanding ACLS Rhythms
Comprehending ACLS rhythms is crucial because it helps healthcare professionals respond quickly and effectively during cardiac emergencies. Here’s why learning ACLS rhythms is so important.
1. Timely Identification Saves Lives
Knowing ACLS rhythms allows responders to quickly recognize the type of cardiac arrest or arrhythmia they’re facing. When you can identify whether it’s ventricular fibrillation, pulseless ventricular tachycardia, or asystole, you can decide the right intervention instantly. This immediate recognition can be the difference between life and death, ensuring patients receive the proper treatment without delaying vital actions like defibrillation or medication.
2. Ensures Appropriate Interventions
Each abnormal rhythm calls for a specific treatment approach. For example, some rhythms require shocks, while others need medication or chest compressions. Understanding these rhythms helps you avoid unnecessary or harmful treatments, guiding you to follow ACLS protocols accurately. This precision means your interventions are more targeted, increasing the chances of a successful outcome.
3. Boosts Confidence in Emergency Situations
When you’re familiar with ACLS rhythms, you’ll feel more prepared during high-pressure scenarios. This confidence helps you stay calm and focused, making better decisions under stress. Instead of second-guessing, you can act decisively, which can improve patient outcomes and reduce your stress during emergencies.
4. Facilitates Team Coordination
In a code situation, the entire team relies on understanding rhythms to work together seamlessly. Recognizing rhythms quickly and accurately allows everyone to agree on the same situation or procedures, whether it’s delivering chest compressions, administering drugs, or defibrillating. This coordination is necessary for effective resuscitation efforts and improving the chances of reviving the patient.
5. Enhances Long-term Patient Care
Understanding rhythms doesn’t just help during the emergency; it also influences ongoing patient care. Recognizing abnormal rhythms early can lead to earlier interventions, potentially reducing brain damage or other complications. Plus, it helps in monitoring patients after resuscitation, ensuring they receive proper follow-up care to prevent future incidents.
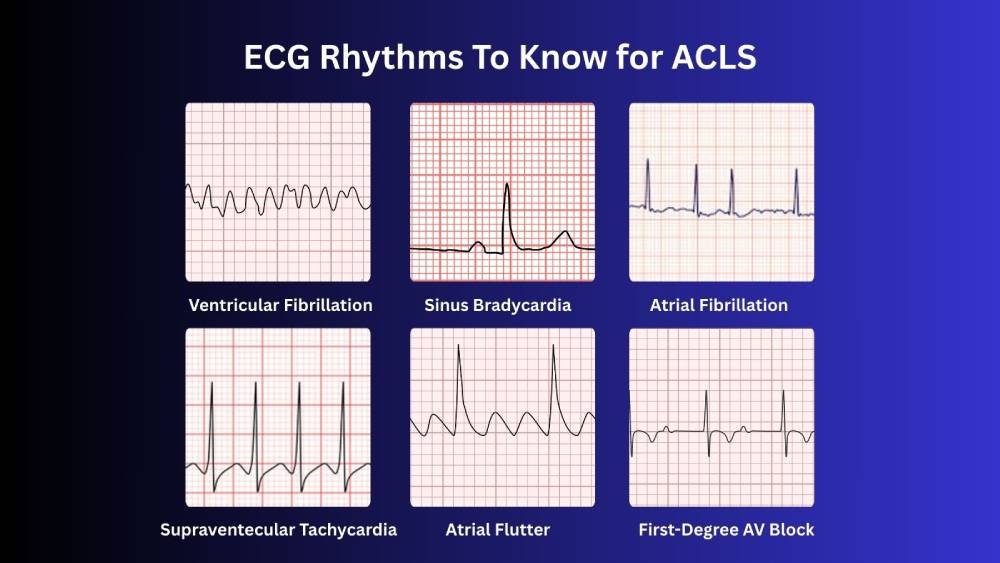
ECG Rhythms to Know For ACLS
The core ACLS rhythms to know are the key arrhythmias encountered during cardiac emergencies, categorized by their shockability and commonality.
1. Shockable Rhythms
Shockable rhythms are types of serious heart arrhythmias that can sometimes be fixed with defibrillation. They are classified into two types. They are mentioned below.
1a. Pulseless Ventricular Tachycardia (pVT)
Pulseless Ventricular Tachycardia (pVT) is a rapid, regular heartbeat originating from the ventricles, but if there’s no pulse, it becomes life-threatening and needs CPR and a defibrillation shock to reset the heart’s rhythm. Medications used in pVT are epinephrine and antiarrhythmics (like amiodarone, lidocaine, and magnesium).
1b. Ventricular Fibrillation (VF)
Ventricular Fibrillation (VF) is when the ventricles quiver (shaking) unpredictably instead of pumping blood, leading to sudden cardiopulmonary arrest. Defibrillation with high quality- CPR is urgent here with medications such as epinephrine and amiodarone to restart the normal rhythm.
2. Non-Shockable Rhythms
Non-shockable rhythms are heart patterns that typically don’t respond to defibrillation. It is classified into two types: ACLS pulseless electrical activity and asystole. They are described below.
2a. Asystole
Asystole is a flatline, with no electrical activity in the heart. It’s a threatening sign, and the focus is on high-quality CPR and medications like epinephrine and vasopressin. Timely recognizing and addressing any reversible conditions, such as hypoxia or significant acidosis.
2b. Pulseless electrical activity (PEA)
Pulseless Electrical Activity (PEA) is when there’s electrical activity in the heart, but no pulse or effective heartbeat. It looks like the heart’s trying to beat, but it can’t produce enough blood to circulate. Treatment involves CPR and addressing the underlying cause such as hypoxia, hypovolemia, hypothermia, or electrolyte imbalances.
3. Bradycardia Rhythms (Slow Heart Rates)
When the heart beats too slowly, some of these may require intervention. Here’s a quick overview of bradycardia rhythms.
3a. Sinus Bradycardia
Sinus bradycardia is a heart rhythm that originates from the sinus node with proper electrical activation of the heart muscle, but at a rate of less than 60 beats per minute (bpm). To diagnose this condition, an electrocardiography must show a normal sinus rhythm with a heart rate below 60 bpm. To increase the heart rate in symptomatic sinus bradycardia, medications atropine, epinephrine, or dopamine are used.
3b. Heart Block
Heart block is a situation where electrical signals in the heart are slowed down or blocked. This involves impaired conduction between the atria and ventricles. It’s categorized by severity.
I. First-Degree AV Block
The electrical signal takes longer than normal to reach the ventricles but still arrives. The electrocardiography shows a prolonged PR interval (>200 ms). It is typically harmless and doesn’t need treatment unless it leads to noticeable symptoms.
II. Second-Degree AV Block / Incomplete Heart Block
Second-degree AV block is a type of atrioventricular conduction delay where some electrical impulses from the atria fail to reach the ventricles, leading to missed heartbeats. It’s divided into two main types.
i. Type I, also called Mobitz Type I or Wenckebach’s AV block
The PR interval gradually lengthens with each heartbeat until a beat (QRS complex) is dropped. This pattern typically indicates a benign conduction delay at the AV node. Patients might be asymptomatic or experience dizziness.
ii. Type II, also called Mobitz Type II
The PR interval remains constant, but occasionally a QRS complex is skipped because the impulse fails to pass to the ventricles. This pattern suggests disease in the His-Purkinje system and can progress to complete heart block. It’s usually more serious and often needs a pacemaker.
III. Third-Degree Heart Block / Complete Heart Block
No relationship between atrial and ventricular activity. The atria beat independently (usually at a normal rate), and the ventricles generate their own slower rhythm. This is a critical condition needing immediate intervention, often with a pacemaker. In emergencies, medications such as atropine or isoproterenol may be used temporarily to raise the heart rate, but they are generally not considered long-term treatments for this condition.
3c. Sick Sinus Bradycardia (Sick Sinus Syndrome)
This is a dysfunction of the sinoatrial node, resulting in abnormal rhythms including sinus bradycardia, sinus pauses, or sinus arrest. It can cause symptoms like dizziness or syncope (fainting or temporary loss) , especially in older patients. Age is a significant risk factor. Other risk factors include high blood pressure, high cholesterol, smoking, and heart disease.
3d. Junctional Bradycardia
Originates from the AV junction, with the rate typically between 40-60 bpm. It occurs when the SA node fails, and the heart’s secondary pacemaker takes over. It might present with a slowed heartbeat and sometimes with features like inverted P waves or absent P waves on electrical heart recording.
3e. Ventricular Bradycardia
Rare, but when the ventricles are the pacing site, the rate drops below 40 bpm. It suggests severe conduction system disease, often associated with underlying structural heart disease or ischemic stroke. It can cause significant symptoms and require urgent treatment.
In summary, bradycardia rhythms can vary from harmless to life-threatening, depending on their origin and severity; each requires a different management approach.
4. Tachycardia Rhythms (Fast Heart Rates)
Here’s a more detailed look at tachycardia rhythms, which are characterized by fast heart rates.
4a. Atrial Fibrillation (AFib)
AFib is an irregular, often rapid heart rhythm originating in the atria. Instead of a coordinated heartbeat, multiple electrical impulses fire unpredictably, causing the atria to quiver. This leads to an irregular ventricular response, which can minimize cardiac efficiency and increase the risk of stroke due to clot formation. Management may include rate control, rhythm control, and anticoagulation.
4b. Atrial Flutter
Atrial flutter involves an immediate, regular atrial rhythm, typically around 250-350 bpm, with a characteristic “sawtooth” pattern on the cardiac electrogram. It results from a re-entrant circuit within the atria. Although the ventricular rate is usually slower, it can still cause symptoms like palpitations or dizziness. Treatment includes medications, cardioversion, and sometimes catheter ablation.
4c. Ventricular Tachycardia (VT)
VT is a rapid heart rhythm originating in the ventricles, usually lasting less than 30 seconds. It can be sustained or unsustained. It may cause dizziness, chest pain, or syncope and can deteriorate into ventricular fibrillation if untreated. The condition is often linked to structural heart diseases, such as cardiomyopathy or scar tissue from a previous infarct. Emergency management may involve antiarrhythmic drugs, cardioversion, or implantation of a defibrillator.
4d. Supraventricular Tachycardia (SVT)
SVT is a fast, regular rhythm that originates above the ventricles, often due to re-entry pathways within the atria or AV node. Rates typically range from 150 to 250 bpm. It causes sudden episodes of palpitations, dizziness, or chest discomfort. Treatment options include vagal maneuvers, medications like adenosine, and sometimes cardioversion if unstable.
4e. Ventricular Fibrillation
VF is a messy and disorganized electrical activity in the ventricles, leading to no effective heartbeat or blood circulation. It is a life-threatening emergency requiring immediate defibrillation to restore a normal rhythm. VF often results in sudden cardiac arrest if not treated promptly.
EKG Rhythms That Can Confuse You on the ACLS Exam
These rhythms can seem similar to other arrhythmias, so careful analysis and correlating findings with clinical context are essential during ACLS assessments. Here’s a quick rundown.
1. Artifact
Artifact refers to false signals on the EKG caused by muscle twitching, patient movement, loose electrodes, or electrical interference. It can mimic or obscure real rhythms, making it seem like there’s an abnormality when there isn’t. Always check the leads and the patient before jumping to conclusions.
2. Idioventricular Rhythm
This rhythm occurs when the ventricles take over pacing the heart, typically with a rate of 20-40 bpm after ROSC. It results from ischemia or severe bradycardia and can look like a slow, wide-complex rhythm. Unlike ventricular tachycardia, it often has a more regular pattern but is less life-threatening unless it deteriorates into asystole.
3. Accelerated Junctional Rhythm
AJR occurs when the heart’s pacemaker shifts to the AV junction, causing it to fire faster than usual (rate of 60-100 bpm). The key features include absent or inverted P waves (since atrial depolarization occurs backwards) and a narrow QRS complex. It can be confused with sinus or V-paced rhythms.
Tips for Improving ACLS Rhythm Analysis Skills
In ACLS, rhythm recognition plays a prominent role in guiding interventions during cardiac emergencies. Here are a few tips for it.
1. Master the Basic ECG Features
Focus on heart rate, rhythm regularity, P wave presence, QRS width, and PR interval. Developing a checklist helps prevent missing details.
2. Use a Step-by-Step Approach
- Step 1: Check if the rhythm is regular or irregular.
- Step 2: Determine if the P waves are present and if they are associated with QRS complexes.
- Step 3: Measure the rate: Is it too slow, normal, or fast?
- Step 4: Assess QRS width: narrow (<120 ms) or wide (>120 ms).
- Step 5: Look for normal or abnormal intervals.
3. Differentiate Shockable from Non-Shockable Rhythms
Shockable rhythms, like ventricular fibrillation and pulseless ventricular tachycardia, respond well to defibrillation and need shocks to restart the heart. Non-shockable rhythms, such as asystole and pulseless electrical activity, don’t benefit from shocks; instead, they require CPR and medicines to support circulation.
4. Practice with Diverse Examples
Use practice EKGs, simulation scenarios, or digital tools. Repeated exposure reinforces recognition patterns.
5. Understand Pathophysiology
The study of how a disease impacts the body’s physiological functions. Knowing the underlying mechanisms helps predict rhythm changes and appropriate interventions.
6. Stay Calm and Focused
During emergencies, stay calm and take a deep breath before doing anything , focus on a methodical approach that reduces errors.
7. Continual Learning
Keep up with updates from ACLS guidelines and review case studies regularly. It will increase your knowledge and make you more confident.
Summary Table of EKG Rhythms For ACLS
Here’s a handy summary table of common EKG rhythms for ACLS, designed to quickly clarify identification and management.
| Rhythm | Shockable | First Line Treatment |
| 1. Ventricular Fibrillation | Yes | AED, CPR, Epinephrine |
| 2. Pulseless Ventricular Tachycardia (pVT) | Yes | AED, CPR, Epinephrine |
| 3. Asystole | No | CPR, Epinephrine |
| 4. Pulseless Electrical Activity (PEA) | No | CPR, Epinephrine |
| 5. Supraventricular Tachycardia (SVT) | No | Vagal Maneuvers, Adenosine |
| 6. Bradycardia (Symptomatic) | No | Atropine, Pacing |
| 7. Atrial Fibrillation | No | Cardioversion, Rate Control |
| 8. Ventricular Tachycardia (VT) | No | Antiarrhythmic, Cardioversion |
Essential ECG Rhythms for Successful ACLS Certification
In short, rapid recognition of arrhythmias and prompt, appropriate responses are vital to improving patient survival during cardiac emergencies. Continuous practice and simulation training help refine these skills, making responders more confident and effective.
Bayside CPR is here to support you with comprehensive courses in PALS, ACLS, BLS, CPR, and First Aid. We also offer group training options, ensuring your organization is fully equipped and prepared to act swiftly when emergencies arise. Visit our training center or contact us to learn more.
Our lifesaving courses combine a brief online lesson with a 30-minute in-person skills session at over 60 locations. Earn your AHA Standard certification and leave with your official card in hand, ready to act.