CPR, or cardiopulmonary resuscitation, is a life-saving technique that helps keep blood and oxygen flowing through the body when someone’s heart stops beating. It incorporates chest compressions with rescue breaths to support circulation and oxygenation. Which prevents brain damage and increases the chances of survival until advanced care arrives.
One of the most critical parts of CPR is managing the airway, making sure oxygen can actually get into the lungs. When an advanced airway like an endotracheal tube or supraglottic device is in place, CPR shifts a bit. The way we deliver breaths and compressions changes to match the continuous support the airway provides.
Let’s break down exactly how those changes work and why they matter so you can feel confident knowing what to do when every second counts.
1. What is an Advanced Airway?
An advanced airway in CPR refers to medical devices that go beyond basic maneuvers like head tilt, chin lift, or jaw thrust. It is a medical device used to keep the airway open and ensure effective ventilation during emergencies like cardiac arrest. It includes tools like ETT or SGAs, which go deeper than basic airway methods such as a head tilt or bag-mask.
Trained professionals, such as paramedics, respiratory therapists, or physicians—are the ones who insert these devices, usually in high-stakes situations where a person can’t breathe on their own. We use an advanced airway to protect the airway from obstruction, deliver oxygen directly to the lungs, and allow for more controlled and secure breathing support. It’s a critical step when basic methods aren’t enough to maintain proper ventilation.
2. When to Insert an Advanced Airway
There are several critical situations where inserting an advanced airway can be life-saving. Knowing when to use one helps ensure the patient gets the oxygen they need while protecting their airway from further harm.
2a. Respiratory Failure
When someone experiences respiratory failure and can’t breathe sufficiently to exchange oxygen into their lungs or remove carbon dioxide, an advanced airway becomes crucial. It provides healthcare providers with a reliable method for delivering oxygen and supporting breathing when the body is unable to do so on its own. This can happen suddenly, like during a severe asthma attack or drug overdose, and acting quickly with the right airway can make all the difference.
2b. Cardiac Arrest
In cardiac arrest, the heart stops pumping blood, and breathing often stops too. As soon as CPR begins, securing an advanced airway allows rescuers to give consistent oxygen while keeping chest compressions going without interruption. It’s especially helpful during prolonged resuscitation efforts when basic airway techniques might not be enough to maintain good ventilation. Understand the ACLS cardiac arrest algorithm and confidently apply it when needed.
2c. Major Trauma
Major trauma, like a car accident or a serious fall, can damage the airway or interfere with breathing. In these situations, inserting an advanced airway early helps prevent complications like swelling, bleeding, or obstruction. It also ensures oxygen can reach vital organs while other injuries are treated. Trauma care often moves fast, so securing the airway early is a top priority.
2d. Altered Consciousness
If someone becomes unconscious or has a reduced level of alertness, they may lose the ability to protect their airway. Their tongue or relaxed muscles can block airflow, and they’re at higher risk of choking. An advanced airway takes over that protective role and keeps the airway open, helping prevent suffocation or aspiration.
2e. High Risk Of Aspiration
Aspiration happens when something like vomit or stomach contents enters the lungs, which can cause serious infections or block airways. If a person is vomiting, unconscious, or has other risk factors, especially during resuscitation, placing an advanced airway can help protect the lungs. It acts as a barrier, keeping harmful materials out and clean air going in.
2f. Surgical Procedures
During many surgeries, especially those that require general anesthesia, doctors use an advanced airway to take full control of the patient’s breathing. Anesthesia can relax the muscles so much that natural breathing stops, and an advanced airway ensures the lungs continue to get oxygen throughout the procedure. It also helps keep the airway protected while the patient is unconscious.
3. When Not to Use an Advanced Airway
While advanced airways can be life-saving, they’re not always the right choice in every situation. Knowing when not to use one is just as important as knowing when to act.
3a. Cervical spine injury: Extra caution is needed when placing advanced airways in patients with possible cervical spine injuries to avoid worsening the damage.
3b. Intact gag reflex: You should avoid inserting an oropharyngeal airway (OPA) in patients who still have a gag reflex, as it can trigger gagging or lead to aspiration.
3c. Alternatives: When standard airway techniques don’t work, alternative methods like cricothyrotomy may be needed to secure the airway and ensure oxygen delivery.
4. Types of an Advanced Airway in CPR
In cardiopulmonary resuscitation, there are two types of advanced airway management devices. They are described below
4a. Endotracheal Tube (ETT)
An endotracheal tube, or ETT, also known as intubation, is one of the most common advanced airways used in emergency and surgical settings. It’s a flexible plastic tube that goes through the mouth or nose and into the windpipe (trachea) to secure the airway directly. Doctors or trained providers insert the ETT using a laryngoscope, which helps them see the vocal cords and guide the tube safely into place. Once positioned, the tube connects to a ventilator or manual bag to deliver oxygen straight to the lungs. The ETT also has a small inflatable cuff that seals the airway, preventing air leaks and stopping anything like stomach contents from getting into the lungs. It provides a very reliable way to control breathing in critical situations.
4b. Supraglottic Airway (SGAs)
A supraglottic airway, or SGA, is another type of advanced airway designed to sit above the vocal cords rather than inside the trachea like an endotracheal tube. Devices like the Laryngeal Mask Airway (LMA) and King Laryngeal Tube (King LT) are popular SGAs. They’re easier and quicker to insert, making them a great option when intubation is difficult or needs to happen fast. SGAs create a seal around the opening of the windpipe, allowing oxygen to flow into the lungs without needing to pass through the vocal cords. While they don’t offer as tight a seal as an ETT, SGAs still provide effective ventilation and airway protection, especially during emergencies or short procedures.
5. Ensuring the Correct Positioning of the Advanced Airway
To ensure an advanced airway works effectively, proper placement is critical. Here are the key steps providers follow to confirm the airway is positioned correctly and stays secure.
1. Visual Confirmation: Use a laryngoscope or direct visualization during insertion to see the airway device pass through the vocal cords.
2. Chest Rise: Observe symmetrical chest rise with each ventilation to confirm air is entering the lungs.
3. Breath Sounds: Listen with a stethoscope over both lungs and the stomach to ensure breath sounds are present in the lungs and absent over the stomach, indicating proper placement.
4. Capnography: Use a carbon dioxide detector (capnograph) to confirm the presence of exhaled CO2, which signals correct tracheal placement.
5. Tube Markings: Check the depth markings on the tube at the teeth or lips to ensure it sits at the appropriate insertion depth.
6. Secure the Tube: Once placement is confirmed, secure the airway device firmly to prevent displacement.
7. Continuous Monitoring: Regularly reassess placement during patient movement or transport to catch any accidental dislodgement early.
6. CPR Technique with an Advanced Airway
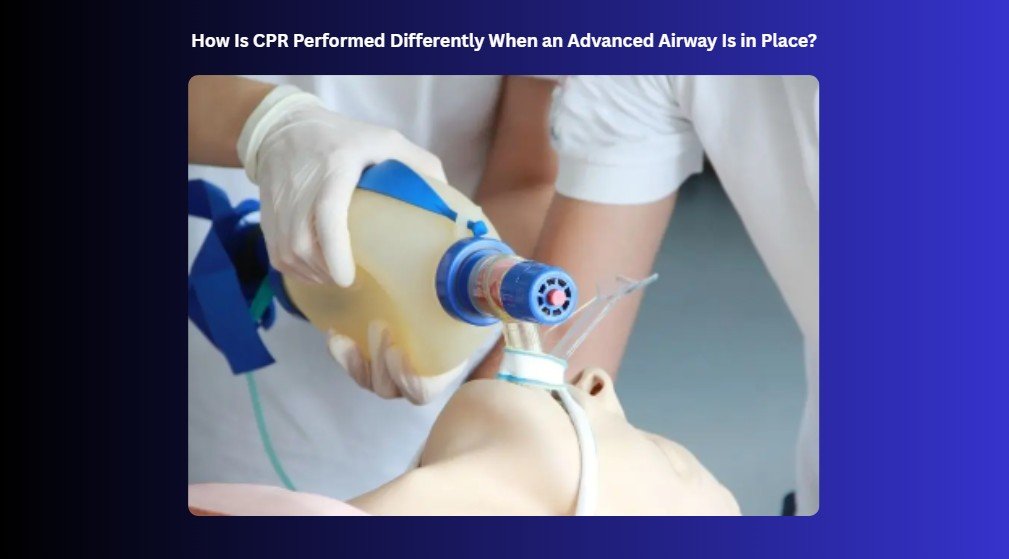
Once an advanced airway is in place (like an ETT or SGA), the approach to CPR changes. Here’s how to properly coordinate ventilations and compressions:
6a. Ventilation Guidelines
- Deliver 1 breath every 6 seconds (10 breaths per minute), continuously.
- Do not pause chest compressions to give breaths.
- Provide only enough air to make the chest visibly rise.
- Avoid over-ventilating, which can increase intrathoracic pressure and reduce blood return to the heart.
- Use a bag-valve mask or ventilator connected to high-flow oxygen.
- Monitor for consistent chest movement and end-tidal CO₂ to confirm effective ventilation.
6b. Chest Compression Guidelines
- Perform continuous chest compressions without interruption for breaths.
- Compress the chest at a rate of 100–120 compressions per minute.
- Push down at least 2 inches (5 cm) deep in adults.
- Allow full chest recoil after each compression.
- Minimize interruptions, even during rescuer switches or breath delivery.
6c. No More Compression-to-Breath Ratio
- When no advanced airway is in place, use a 30:2 compression-to-breath ratio.
- Once an advanced airway is secured, switch to continuous compressions with 1 breath every 6 seconds, without synchronizing the two.
7. Perform High-Quality CPR
Performing high-quality CPR means focusing on a few key actions that give someone the best chance of survival. Here’s how to perform high-quality CPR :
- Place hands in the center of the chest, on the lower half of the breastbone.
- Push hard and fast, compressing about 2 inches (5 cm) deep in adults.
- Allow full chest recoil between compressions.
- Maintain a compression rate of 100 to 120 compressions per minute.
- Minimize pauses in compressions, especially during breaths or rescuer switches.
- Give rescue breaths that last about 1 second each, making the chest rise visibly.
- Avoid over-inflating the lungs with breaths.
- Stay calm and focused to keep compressions strong and consistent.
- Continue CPR until professional help arrives or the person shows signs of life.
Advanced Airway Management During CPR
In summary, how CPR changes with an advanced airway in place can make a huge difference when every second counts. By knowing when to insert one, how to confirm it’s working, and how to adjust your compressions and breaths accordingly, you’re better prepared to act with confidence in high-stress situations. Continuous compressions paired with steady, controlled ventilations help maintain oxygen and blood flow when the body can’t do it on its own. It’s all about working smarter, staying focused, and giving someone the best possible chance at survival.
Prepare for critical moments the smart way with Bayside CPR. Finish a short online course, then complete a 30-minute, hands-on skills session at one of our 60+ convenient locations. You’ll earn your AHA Standard ACLS, BLS, PALS, CPR, or First Aid certification and leave the same day fully certified, confident, and ready to respond.
Also Read: Facts & Myths Of CPR