Even though it’s commonly written as “Ambu,” do you know what it stands for? It means “artificial manual breathing unit” and refers to bag-valve masks (BVMs). The name is shortened to Ambu because the original Ambu bag was developed by a company called Testa Laboratory, which later rebranded as Ambu in the 1980s.An Ambu bag is a handheld manual resuscitation device that helps a person breathe when they are not breathing adequately or have stopped breathing. It works by delivering air or oxygen into the lungs through a self-inflating bag attached to a face mask or advanced airway. Because of this, Ambu bags are a key tool for airway management and ventilation during CPR, cardiac arrest, respiratory failure, and emergency resuscitation in both prehospital and hospital settings.
Key Components of an Ambu Bag
An Ambu bag consists of several essential parts that work together to deliver effective ventilation:
- Self-Inflating Bag: A squeezable bag that pushes air or oxygen into the lungs.
- Face Mask: Creates a seal over the nose and mouth to deliver ventilation.
- One-Way Valve: Prevents exhaled air from re-entering the bag.
- Oxygen Inlet Port: Allows connection to supplemental oxygen.
- Oxygen Reservoir (if present): Increases the concentration of delivered oxygen.
- Exhalation Port: Allows carbon dioxide to escape during exhalation.
Each component plays a critical role in ensuring safe and effective ventilation during CPR.
How Ambu Bags Work: Delivering Ventilation
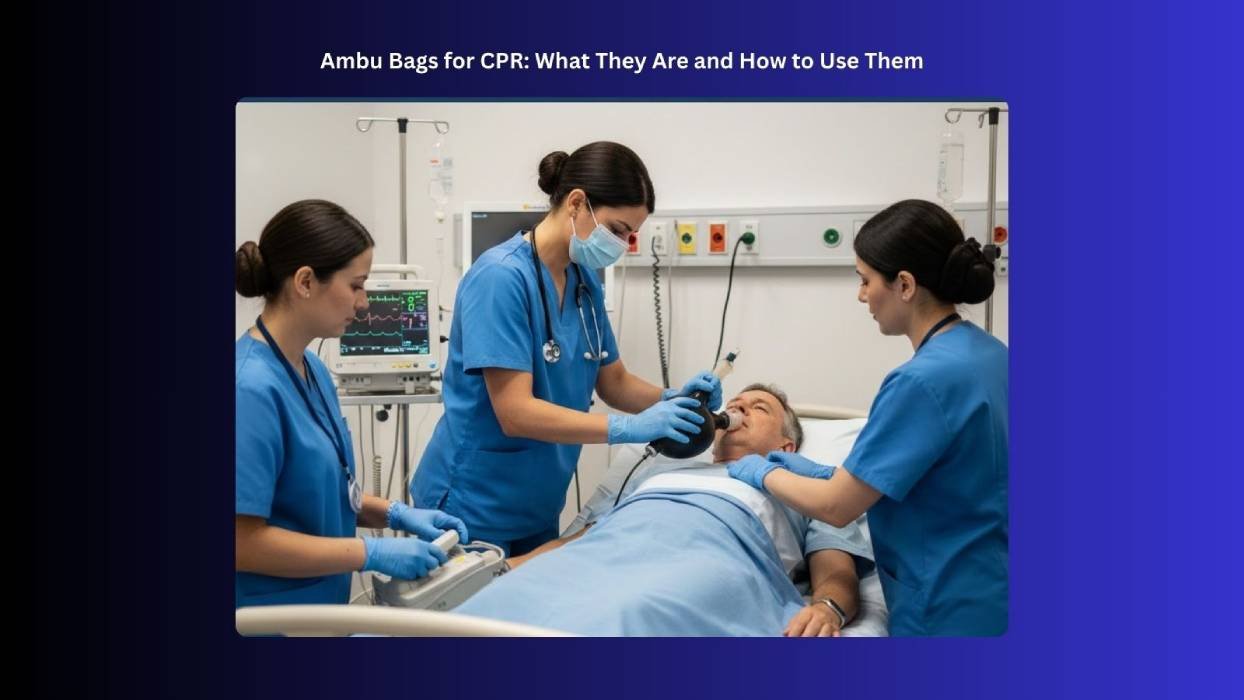
An Artificial Manual Breathing Unit (Ambu) bag delivers ventilation through manual positive-pressure breaths, allowing the rescuer to support or replace a patient’s breathing. Learning the correct technique for bag-mask ventilation ensures effective breaths and optimal ventilation during CPR.
- Airway Positioning and Mask Seal: Clear the airway, position the head, and create a tight seal over the nose and mouth.
- Bag Compression: Squeeze the bag to push air or oxygen into the lungs, producing a visible chest rise.
- Automatic Refill: Release the bag to let it self-inflate, drawing in fresh air or oxygen.
- Exhalation: The patient passively exhales through the exhalation port.
During CPR, ventilations are carefully timed to minimize interruptions in chest compressions, delivering just enough volume to produce a visible chest rise and avoid over-ventilation.
Why Ambu Bags Are Used During CPR
Ambu bags are essential tools for rescuers because they:
- Provide Effective Ventilation: Deliver positive-pressure breaths to patients who are not breathing effectively.
- Enhance Oxygen Supply: When connected to supplemental oxygen, they can deliver nearly 100% oxygen, reducing the risk of brain injury.
- Improve Rescuer Safety: Act as a barrier, minimizing exposure to saliva, breath, and bodily fluids.
- Offer Temporary Respiratory Support: Maintain oxygenation until the patient can breathe independently or an advanced airway is established.
When to Use an Ambu Bag
Use an Ambu bag whenever someone cannot breathe on their own:
- Patient Isn’t Breathing: Supports ventilation for apnea or weak, irregular breaths.
- During Cardiac Arrest: Complements chest compressions to maintain oxygen delivery.
- Airway Compromise: Keeps air flowing when obstructions, swelling, or injuries block normal breathing.
- Before Advanced Airway Support Arrives: Provides immediate ventilation until intubation, mechanical ventilation, or advanced care is available.
How to Use an Ambu Bag During CPR
CPR works best when breaths and chest compressions are done correctly. Using an Artificial Manual Breathing Unit (AMBU) bag the right way helps get oxygen to the patient quickly and safely.
1. Preparing the Ambu Bag
- Inspect for damage, airflow issues, or valve problems.
- Connect oxygen if available.
- Choose a properly sized mask for the patient.
2. Mask Selection and Seal
- Select a mask that fits the patient’s age and face.
- Use the E-C hand technique to lift the jaw and maintain airway patency.
- Confirm a visible chest rise for effective ventilation.
3. Ventilation Technique
- Squeeze the bag gently until the chest rises, then allow it to refill.
- Avoid over-ventilation and gastric inflation.
4. Ventilation Rates
- Adults with advanced airway: 1 breath every 6 seconds (~10 breaths/min).
- Children/Infants with advanced airway: 1 breath every 2–3 seconds (~20–30 breaths/min).
- Single rescuer without advanced airway: Adults: 30:2 compressions to breaths; Children/Infants: 30:2 (single rescuer), 15:2 (two rescuers).
5. Coordinating With Chest Compressions
- With an advanced airway: Continue compressions, give breaths on schedule.
- Without an advanced airway: Pause briefly to deliver 2 effective breaths.
6. Two-Rescuer CPR
- One rescuer performs chest compressions.
- The second rescuer handles the Ambu bag.
- Clear communication ensures timing and quality of ventilation.
Common Mistakes and Safety Tips
Using an Artificial Manual Breathing Unit (AMBU) bag during CPR can save lives, but mistakes happen more often than you think. Knowing the common errors helps you give air effectively and keep the patient safe.
- Improper Mask Seal: Air leaks reduce ventilation; always use the E-C technique.
- Over-Ventilation: Can cause gastric inflation or reduced circulation; give slow, steady breaths.
- Under-Ventilation: Shallow breaths reduce oxygenation; ensure visible chest rise.
- Incorrect Bag Squeezing: Avoid squeezing too fast; aim for ~1 second per breath.
- Neglecting Airway Position: Always perform head tilt–chin lift or jaw thrust to open the airway.
Special Considerations When Using an Ambu Bag
Using an Artificial Manual Breathing Unit (AMBU) bag safely means paying attention to a few important details. Following these tips helps patients get the oxygen they need and prevents problems during emergencies.
- Supplemental Oxygen: Connect securely; use 10–15 L/min flow.
- Advanced Airways: Deliver steady ventilation without pausing compressions.
- Airway Obstruction & Gastric Inflation: Use correct maneuvers and controlled breaths to prevent complications.
Ambu Bag Use in Emergency and Clinical Settings
Artificial Manual Breathing Unit (AMBU) bags help people breathe when they cannot do so on their own. Learning to use them correctly can save lives in emergencies and everyday hospital care.
- Prehospital (EMTs/Paramedics): Provide temporary respiratory support during transport, cardiac arrest, or trauma.
- Hospital/Code Blue: Rapid oxygenation during emergencies, ICUs, EDs, or operating rooms until advanced airway placement.
- CPR Training: Hands-on practice with bag-valve masks improves ventilation technique, mask seal, and rescuer confidence.
Key Takeaways for Using an Ambu Bag During CPR
In summary, using an Ambu bag might feel tricky at first, but with practice, it becomes a powerful tool to help someone breathe when they can’t do it themselves. By making a proper seal, giving steady breaths, and coordinating with chest compressions, you can deliver oxygen safely and effectively. Remember, the key is calm, controlled ventilation; each squeeze of the bag can make a real difference. With knowledge, skill, and confidence, you can provide life-saving support whenever it’s needed.
Sign up for a CPR class today with Bayside CPR and take charge of emergency readiness. Start with a short online course, then attend a 30-minute in-person skills session at any of our 60+ locations, scheduled to fit even the busiest lifestyles. After completing both parts, you’ll receive your official AHA course completion card the same day, fully trained and ready to act when it matters most. We also offer BLS, ACLS, and PALS classes.