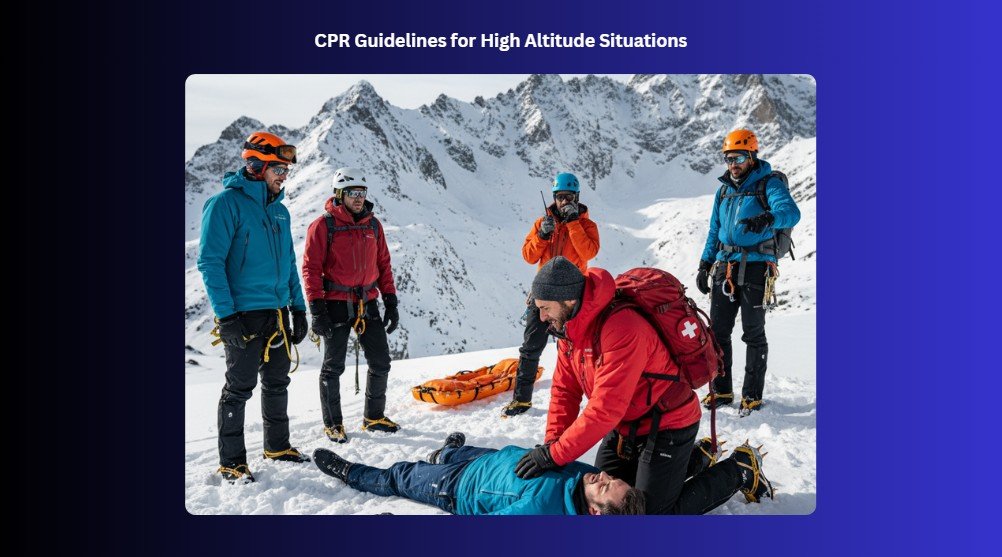
Going to high-altitude areas like snowy mountains, green hills, or remote trails can be exciting, but it also comes with unique risks. Accidents or sudden health emergencies can happen far from help, and sometimes there is little to no phone signal. Knowing how to respond with CPR (cardiopulmonary resuscitation) in these situations can make a huge difference. The air is thinner, your body works differently, and conditions can change quickly, so standard emergency steps might need small adjustments. Being prepared, staying calm, and acting confidently can help keep someone safe until professional help arrives. This guide is here to help rescuers adjust their approach and stay effective when giving life-saving care in the mountains or at high elevations.
Definition of High Altitude
High altitude refers to places far above sea level where the air is thinner and contains less oxygen. As elevation increases, breathing becomes harder, and the body needs time to adjust. People often notice this change when visiting mountains or high plains. Understanding what high altitude means helps you prepare your body and stay healthy when exploring or traveling to these elevated places.
Altitude Classifications:
Altitude classifications help you understand how different height levels affect your body. Knowing these levels makes it easier to prepare and stay healthy when traveling to higher places.
- High Altitude: 8,000 to 12,000 feet (2,438 to 3,658 meters).
- Very High Altitude: 12,000 to 18,000 feet (3,658 to 5,487 meters).
- Extreme Altitude: 18,000+ feet (5,500+ meters).
Physiological Effects of Altitude
When you travel to high places, your body faces new challenges as the air gets thinner. Let’s look at how altitude affects your body in different ways.
1. Lower Oxygen Availability
As you climb higher, the air contains less oxygen, so your body gets less of the fuel it needs. You may notice that simple activities feel harder, and your muscles tire more quickly. Your body has to work harder to keep everything running smoothly.
2. Acute Mountain Sickness (AMS)
At high altitudes, some people feel headaches, nausea, or dizziness. This is called acute mountain sickness, and it happens when your body struggles to adjust to the thinner air. Taking it slow and giving yourself time to adapt can make a big difference.
3. Increased Breathing and Heart Rate
To cope with lower oxygen, your breathing speeds up and your heart beats faster. This helps your body get more oxygen to your organs and muscles. You may notice yourself breathing more deeply or feeling your heart race even when resting.
4. Dehydration Risk and Fluid Balance Changes
High places can dry out your body faster, causing you to lose water without noticing. You may feel thirsty more often, and your body needs more fluids to stay balanced. Drinking water regularly helps prevent headaches and fatigue.
5. Impaired Sleep and Cognitive Function
Altitude can make it harder to sleep well, leaving you tired and foggy during the day. Your thinking may slow down, and concentrating on tasks can feel tougher. Simple rest, hydration, and pacing yourself help your mind and body adjust.
Common Causes of Cardiac Arrest at High Altitude
Being at high altitudes puts extra stress on your heart and lungs. Certain conditions can suddenly make your heart stop if you’re not careful.
- Hypoxia and Acute Mountain Sickness (AMS): At high altitudes, your body may not get enough oxygen, which can make your heart work harder. This lack of oxygen can trigger serious problems, including sudden cardiac arrest.
- High-Altitude Pulmonary Edema (HAPE): Fluid can build up in your lungs when you climb too high, too fast. This makes it hard to breathe and can put extreme stress on your heart.
- High-Altitude Cerebral Edema (HACE): Swelling in the brain can happen at high elevations, causing confusion and severe headaches. If untreated, it can lead to life-threatening heart complications.
- Trauma, Hypothermia, or Exertional Exhaustion: Falls, cold exposure, or extreme tiredness can overwhelm your body at high altitudes. These stresses can stop your heart if not managed quickly.
- Pre-Existing Cardiac Conditions Exacerbated by Altitude: Heart problems you already have can get worse when oxygen is low and the body works harder. This can increase the risk of sudden cardiac arrest.
Also, Read: Reversible Causes of Cardiac Arrest: Hs and Ts
Key Challenges in Performing CPR at Altitude
Performing CPR at high altitude brings unique challenges that make saving a life harder. The thin air, tough weather, and tricky terrain can quickly tire rescuers and limit resources.
- Limited Oxygen Availability: At high altitudes, the air has less oxygen, which makes it harder for both the patient and the rescuer. The heart and brain get less oxygen, so CPR may need extra effort and focus to keep the patient alive.
- Rescuer Fatigue Due to Thin Air: The thin air can tire rescuers much faster than at sea level. Even strong, trained helpers may feel short of breath quickly, which can slow down chest compressions and make sustained CPR more difficult.
- Harsh Environmental Conditions: Cold, wind, and uneven ground can make performing CPR tricky. Rescuers may slip, shiver, or struggle to keep the patient warm, all of which can affect how well life-saving care is delivered.
- Delayed Access to Advanced Medical Support: Getting help from hospitals or paramedics takes longer at high altitudes. This delay means rescuers must provide care for longer, sometimes without guidance, which can add stress and increase risk for both patient and helper.
- Equipment Limitations: Carrying and using equipment like defibrillators or oxygen tanks is harder on rough terrain. Limited or heavy gear can slow down care, and sometimes critical tools may not be available at all.
Steps of CPR At High Altitude
CPR saves lives, even when you’re high up in the mountains. Knowing the right steps can help you act quickly and confidently.
Step 1: Initial Assessment and Safety
Before you do anything, make sure the area around you is safe. Check for falling rocks, slippery surfaces, or other hazards common at high altitudes. Approach the person carefully and see if they respond by tapping their shoulder and calling their name. If they do not respond and are not breathing normally, it is time to act. Quickly call for help or have someone contact emergency services while you get ready to start CPR. You can also play CPR songs to help you stay on beat, ensuring your compressions remain consistent and effective.
Step 2: Chest Compressions
Place the heel of one hand in the center of the chest and the other hand on top. Keep your arms straight and shoulders above your hands. Push hard and fast, letting the chest rise fully between compressions. Aim for a steady rhythm, about 100 to 120 compressions each minute. At high altitudes, your energy may tire faster, so focus on keeping a strong, consistent pace. To maintain that rhythm and minimize interruptions, it helps to understand how you can achieve a high chest compression fraction, a key factor in improving survival rates during CPR.
Step 3: Rescue Breaths and Airway Management
After 30 compressions, open the person’s airway by tilting the head back and lifting the chin. Pinch the nose closed, cover their mouth with yours, and give 2 slow breaths. Watch for the chest to rise with each breath. Rescue breaths provide oxygen that keeps organs alive until professional help arrives.
Step 4: Hands-Only CPR
If you feel uncomfortable giving breaths, focus on chest compressions only. Push hard and fast in the center of the chest without stopping. Hands-only CPR can keep blood flowing to the brain and heart until help arrives or an AED is ready. It is still very effective, especially when physical conditions make rescue breaths difficult.
Also, Read: Hands-Only CPR vs. Traditional CPR: Key Differences
Step 5: Continue and AED Use
Keep performing CPR and follow any instructions from an automated external defibrillator (AED) if one is available. Turn it on, attach the pads to the chest, and let it analyze the heart rhythm. Follow the voice prompts exactly. Stop compressions only when the AED tells you to, the person starts breathing normally, or trained help arrives.
Step 6: Transport the Victim
Once emergency responders arrive or the person shows signs of life, help move them carefully to a safer location if needed. Continue monitoring breathing and pulse until professionals take over. At high altitude, try to keep the person warm and calm, since cold and stress can worsen their condition. Your care during transport can make a big difference in their recovery.
Rescuer Considerations at High-Altitude
When working at high altitudes, your body faces extra stress and needs extra care. Paying attention to yourself and your team can keep everyone safe and strong.
- Recognize Early Signs of Altitude Sickness in Yourself: Pay close attention to how your body feels as you climb. Headaches, dizziness, or feeling unusually tired are warning signs. Stop, rest, and breathe slowly if you notice anything unusual. Acting early can prevent serious problems.
- Work in Teams, Assign Roles, and Rotate Often: Teamwork keeps everyone safe and organized. Give each person a clear job and switch tasks regularly. This prevents one person from getting too tired and helps the team move smoothly together.
- Monitor Your Own Oxygen Saturation If Possible: If you have a device, check your oxygen levels often. Low oxygen can sneak up on you without obvious symptoms. Watching your numbers helps you adjust pace, rest, or take action before it becomes dangerous.
- Manage Exertion and Hydration to Prevent Exhaustion: Take breaks and drink water regularly as you move. Pushing too hard can drain your energy and make altitude sickness worse. Move at a steady pace and keep your body fueled to stay strong.
Prevention and Preparedness
Proper preparation can significantly reduce the risk of cardiac emergencies and improve outcomes if they occur. Key strategies include.
1. Acclimatize Gradually
- Ascend (climb) slowly to allow the body to adjust to lower oxygen levels.
- Follow the “climb high, sleep low” principle to reduce the risk of acute mountain sickness (AMS).
- Monitor yourself and team members for early symptoms such as headache, nausea, dizziness, or shortness of breath.
2. Carry Essential Equipment
- Bring portable oxygen for emergencies, along with masks or nasal cannulas.
- Pack a basic first aid kit and CPR gear, including gloves, face shields, and automated external defibrillators (AEDs) if possible.
- Ensure all equipment is checked and fully functional before the trip.
3. Train Rescuers in Altitude-Specific Emergency Care
- Conduct refresher courses in high-altitude physiology and wilderness CPR.
- Practice performing CPR in challenging terrain and low-oxygen environments.
- Train team members to recognize altitude-related complications such as HAPE and HACE.
4. Have a Clear Rescue and Evacuation Plan
- Identify safe routes for evacuation and possible landing zones for helicopters if needed.
- Establish communication protocols, including radios, satellite phones, or GPS devices.
- Assign roles in advance so every team member knows their responsibilities during an emergency.
CPR at High Altitude: Stay Ready, Act Confidently
High-altitude CPR is challenging, but with the right preparation and approach, it can save lives. Understanding how thin air affects your body and the person in need helps you act more confidently. Paying attention to safety, pacing yourself, and working closely with your team make a big difference in difficult conditions. By learning altitude-specific techniques, carrying essential equipment, and watching for early signs of trouble, you can stay strong while giving effective care. Every step you take, from compressions to monitoring, helps keep blood and oxygen flowing until professional help arrives, giving the best chance for survival in the mountains.
Stay ready when it matters most with Bayside CPR’s flexible, time-efficient lifesaving courses. Suitable for busy schedules, our training combines a short online module with a quick 30-minute in-person skills check at any of our 60+ locations. Complete your American Heart Association (AHA) training in BLS, ACLS, PALS, CPR, or First Aid and receive your official course completion card the very same day.